
THE MOST SERIOUS complication of contact lens wear to correct refractive error is microbial keratitis (MK). Infections can result in significant corneal scarring, which in some cases reduces best-corrected visual acuity secondary to irregular astigmatism and opacification. The following case reports show that MK can also occur in our medically necessary specialty lens patients.
CASE #1
A 35-year-old male patient who has keratoconus and long-term scleral lens use reported on an emergent basis complaining of a red, painful left eye for three days. He initially went to an urgent care facility, where he was diagnosed with an eye infection and prescribed moxifloxacin b.i.d. OS. His visual acuity with correction OS was hand motion vision.
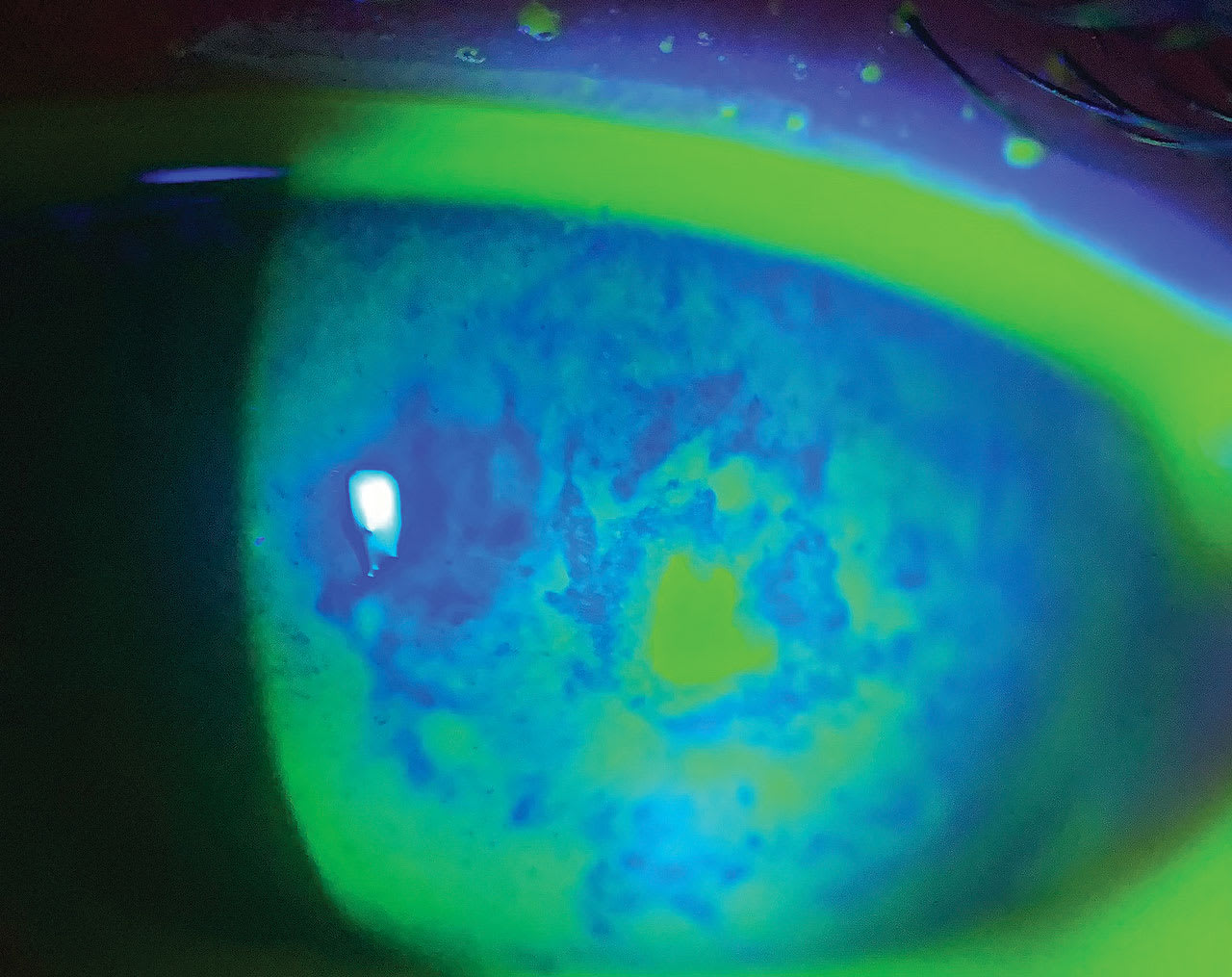
Slit lamp exam showed reactive ptosis, moderate conjunctival injection, corneal scarring, central infiltrative epithelial defect (Figure 1), and trace hypopyon. He was referred to a corneal specialist who diagnosed microbial keratitis. A corneal scraping was performed for culture and the patient was prescribed fortified vancomycin and fortified tobramycin to be used alternately every 30 minutes while awake.
The next day, he had slightly improved and was prescribed bacitracin-polymyxin B ointment at bedtime in addition to the fortified antibiotics. Two days later the tests for cultures were without growth, and he continued to improve. The fortified antibiotics were scaled back to four times per day. One week later, he had no ulceration or infiltrate but did have a hazy scarred area.
The patient was taken off the fortified antibiotics and prescribed prednisolone 1% six times per day. Finally, two weeks later, his uncorrected vision had improved to 20/400 and he was advised to discontinue the ointment and taper off the prednisolone, then recheck for scleral lens reevaluation.
CASE #2
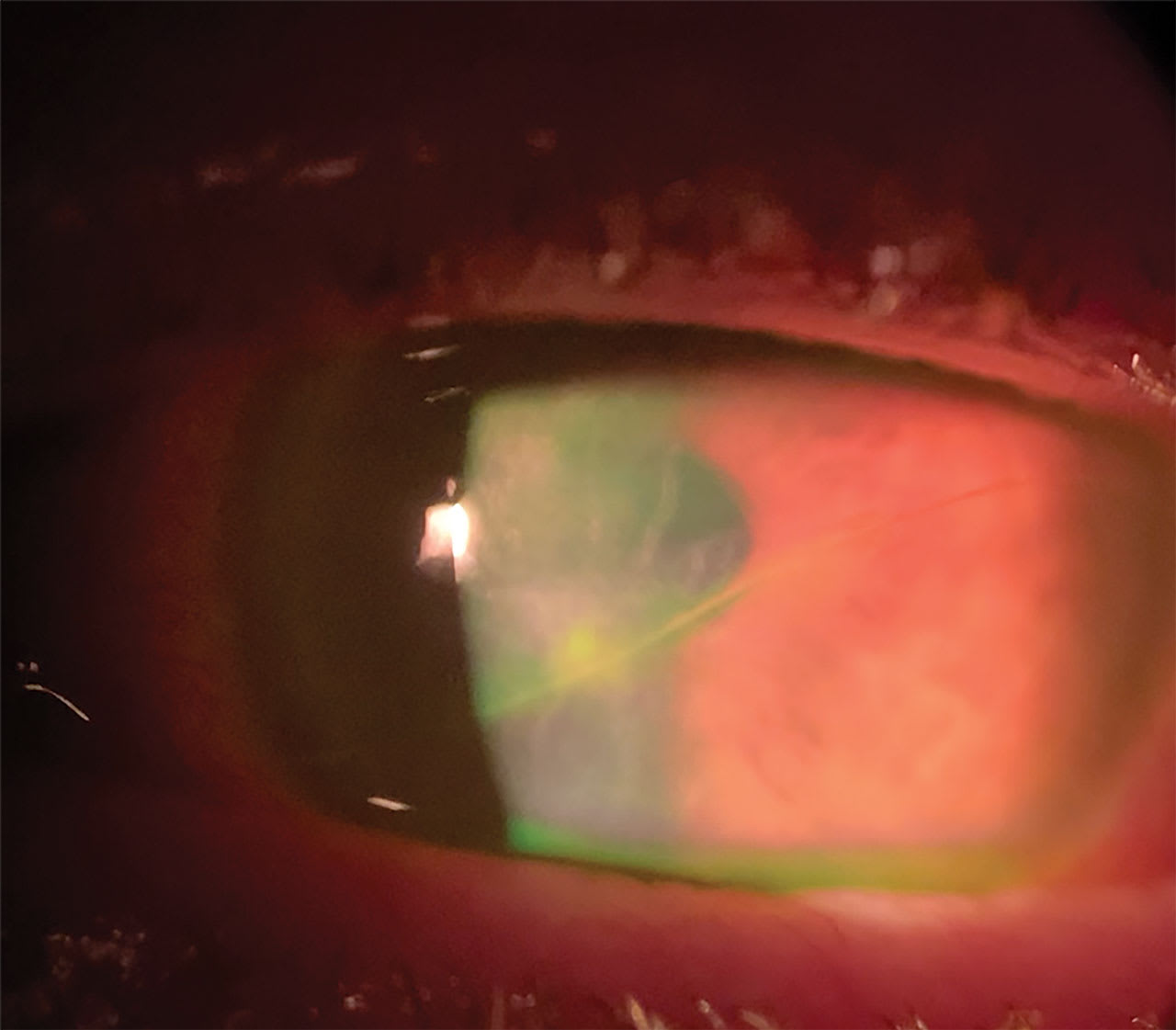
A 76-year-old male who had a history of irregular corneas secondary to anterior basement membrane dystrophy wore scleral lenses for visual improvement. The patient reported urgently with complaints of blurred vision, redness, and mattering of his left eye. His uncorrected vision was 20/400 and slit lamp examination showed a paracentral epithelial defect (Figure 2) with infiltrate, as well as significant corneal edema.
Corneal scraping for culture was performed and the patient was put on fortified vancomycin and tobramycin four times per day. Two days later, the culture came back positive for Staphylococcus and Bacillus bacteria. The epithelial defect and infiltrate were diminished, and the patient was scheduled back four days later.
At the next follow-up, his ulceration and infiltrates were resolved, but he did have some mild scarring. The patient was advised to discontinue the fortified antibiotics and prescribed prednisolone six times per day, which was tapered after 10 days of use. One month later, his uncorrected visual acuity had improved to 20/30 and he successfully returned to scleral lens wear.
It is critical to properly educate specialty lens patients about proper hygiene, solutions, and risk of MK. They should know to immediately discontinue lens wear and report for evaluation if they have signs or symptoms of MK. CLS



