
SCLERAL LENSES have evolved tremendously over the last decade. They provide practitioners with the opportunity to rehabilitate vision for those who, at times, have very few other options for vision correction. With that said, there are several intricacies that exist in the landing zone that can either create success or failure in the scleral fitting process for our patients. Additionally, more is known regarding the shape of the sclera providing physicians more power when fitting scleral lenses.The goals of this article are to review intricacies of the sclera and how to optimize the fitting process.
WHAT WE KNOW ABOUT THE SCLERA
There was a point in time in which scleral lenses were fit using solely spherical landing zone characteristics. There were no differences in the curve of the lens in the landing zone.This resulted in several landing zone attributes that were less than ideal—including impingement and edge lift in certain regions of the lens-conjunctival interface—while some portions of the lens were well aligned and without these fitting challenges.
As a professional community, it was realized that most of the scleral shapes being fitted were not spherical but had some level of irregularity to their shape. Advances in ocular surface measurement technologies now allow eyecare professionals to measure the shape of the ocular surface to provide more information on scleral profile.
The level of irregularity that exists in the scleral shapes of the patients that we are fitting has been demonstrated; in fact, several years ago, DeNaeyer and colleagues measured the scleral shape of 140 eyes in for scleral lens fittings and found the following breakdown of scleral shape: 5.7% were spherical, 28.6% were toric-regular, 40.7% had asymmetric high or low points, and 26% had periodicity different from 180º.1
This has resulted in several advancements in how we select lenses to fit for our patients. Impression molding provides an opportunity to create a lens for an irregularly shaped sclera by taking a mold of the eye and sending the mold to a laboratory for analysis and production of a lens that matches the precise scleral shape of the eye.2,3 Advanced scleral technology now provides clinicians with the opportunity to quantify scleral toricity and order customized lens designs.4
Ultimately, whatever lens is selected for the eye must be assessed for appropriate fitting characteristics. This is performed at the slit lamp and utilizes more advanced technologies. Here we will explore the details of assessing the landing zone to optimize fitting characteristics of the lens.
ANATOMY OF THE LANDING ZONE
The landing zone of a scleral lens has important components that need to be identified to communicate fit characteristics of the lens. The landing zone is defined as the portion of a lens that is intended to fit along the bulbar conjunctiva and underlying sclera in the region outside of the cornea. The landing zone size will vary depending on the manufacturer and the diameter of the lens.
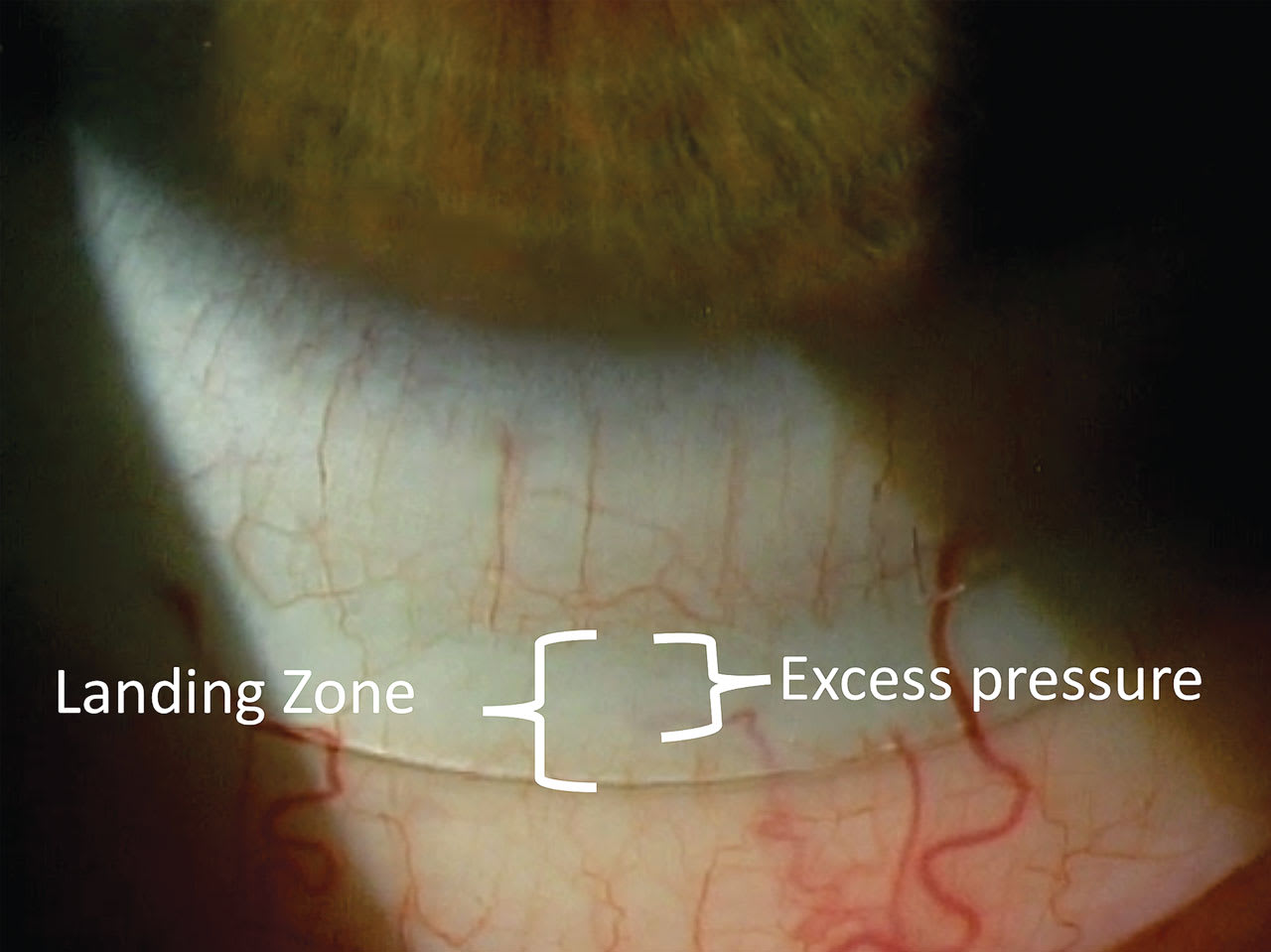
An ideal fitting landing zone will evenly disperse the lens onto the conjunctival surface all the way around the lens. In this instance, there will be no visible blanching that is present in any regions of the landing zone. If there are regions of the landing zone that are uneven with the underlying conjunctiva and sclera, the sclera that is subject to more pressure from the lens can manifest vascular blanching.
When evaluating the landing zone of a scleral lens, there are two main components to view.This analogy is often used to describe the landing zone: If the landing zone is considered a foot, there would be a toe and a heel. The toe is considered the most distal portion of the landing zone from the center of the lens. The heel is considered the more proximal portion of the landing zone to the center of the lens.
Thus, a toe-down relationship in a landing zone would essentially be describing a scleral landing zone in which the trajectory of the landing zone in that region is steeper than the trajectory of the sclera.Another way to describe this would be that the most distal portion of the landing zone is digging into the conjunctival tissue.In extreme examples, vascular blanching in the affected region may be observed.
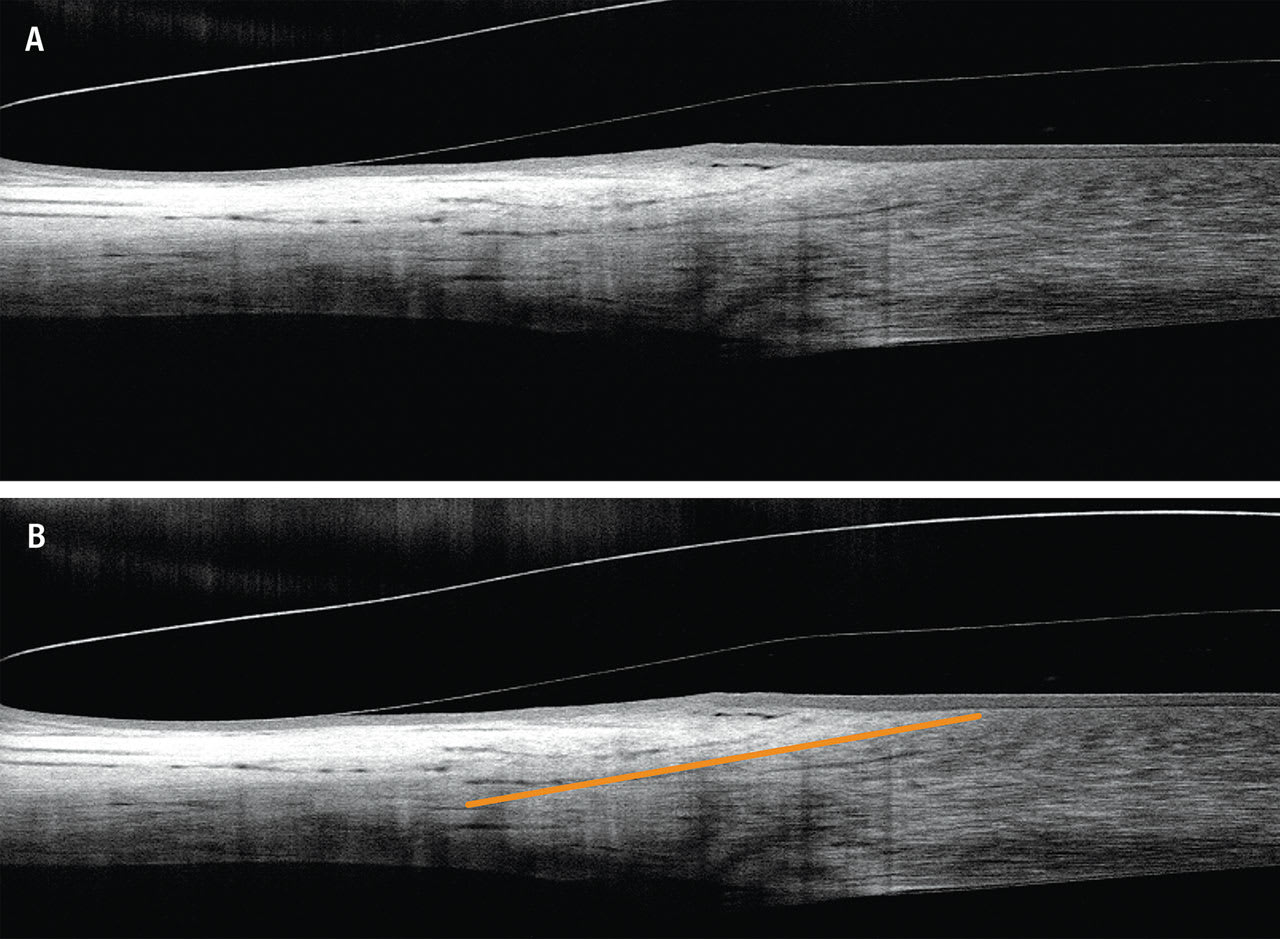
The toe could also be up. In this instance, the trajectory of the landing zone is flatter than that of the scleral profile. Another way to describe this is that the most distal portion of the landing zone is elevated. In extreme examples, vascular blanching may be observed in the heel region (the proximal portion) of the landing zone (Figure 1).
WHY IS CENTRAL CLEARANCE IMPORTANT?
Corneal clearance of a scleral lens describes the distance from the posterior surface of the lens to the anterior surface of the cornea. With that said, there is much more information about the overall fit that we can determine from central corneal clearance than simply that one measurement.
The importance of the vertical scan is often overlooked in the fitting process. This one scan can provide guidance on how vertically centered a lens is fitting.Although there are several factors that can determine the vertical centration of a lens (i.e., greater central apical clearance, scleral shape),5 the landing zone also plays a critical role in this.
If the corneal clearance of the lens demonstrates an even level of clearance superiorly and inferiorly, this lens is well-aligned vertically. If a vertical cross-section through the lens is measured and there is less clearance superiorly than inferiorly, the lens is sitting inferiorly and is not centered.
Although this can occur for several reasons, the landing zone is one of the main culprits for this fitting characteristic and should be examined very closely. This often occurs because the landing zone of the lens is flatter than the trajectory of the sclera (Figure 2). This can also be noted at the slit lamp and observed with or without the use of fluorescein in the bowl of the lens.
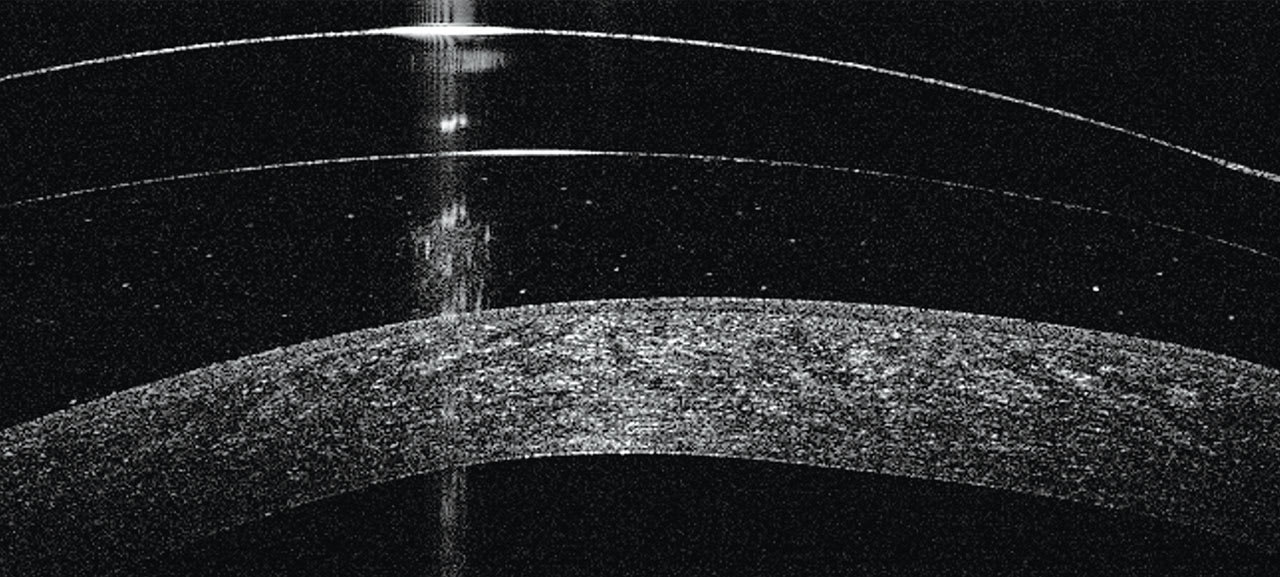
Using this logic, a horizontal cross section of the lens can also be measured to determine lens decentration. The lens will be decentered in the direction of the greater corneal clearance.
CLEARING THE LIMBUS
Before discussing the intricacies of the landing zone, it is very important to understand the limbal region and identify the clearance of a scleral lens in that region. The limbal region contains the stem cells of the cornea, and it is critical to respect their role in adequate corneal health and physiology.As such, it is important to identify limbal clearance and assure that it is present.
One way to assess for limbal clearance is to view the lens on the eye at the slit lamp after fluorescein has been placed into the bowl of the lens. In a fit that adequately clears the cornea, fluorescein should be present in the limbal region of the cornea. There are times when it may be difficult to determine whether there is clearance, as fluorescein is only visible at a minimum thickness of 15µm.6 Additionally, if a patient is coming in for a follow-up visit with the lenses in, they will not have fluorescein in the bowl of the lens, so one cannot determine whether there is limbal clearance after a day of lens wear.
Optical coherence tomography (OCT) provides a viable means of assessing the limbal region and whether either limbal clearance or bearing is present. It is important to identify the limbal region of the cornea in the OCT scan to assure clearance is present. This can be challenging as the epithelium on the cornea is continuous with the conjunctival epithelium. But several visual cues can help identify the limbal region.
The corneal epithelium is highly organized and is clearly different in appearance from the conjunctival epithelium (Figure 3). When you look for the region of transition between the two epithelial surfaces, you can clearly see where they transition from one to another (Figure 4). This is the limbal region.7,8
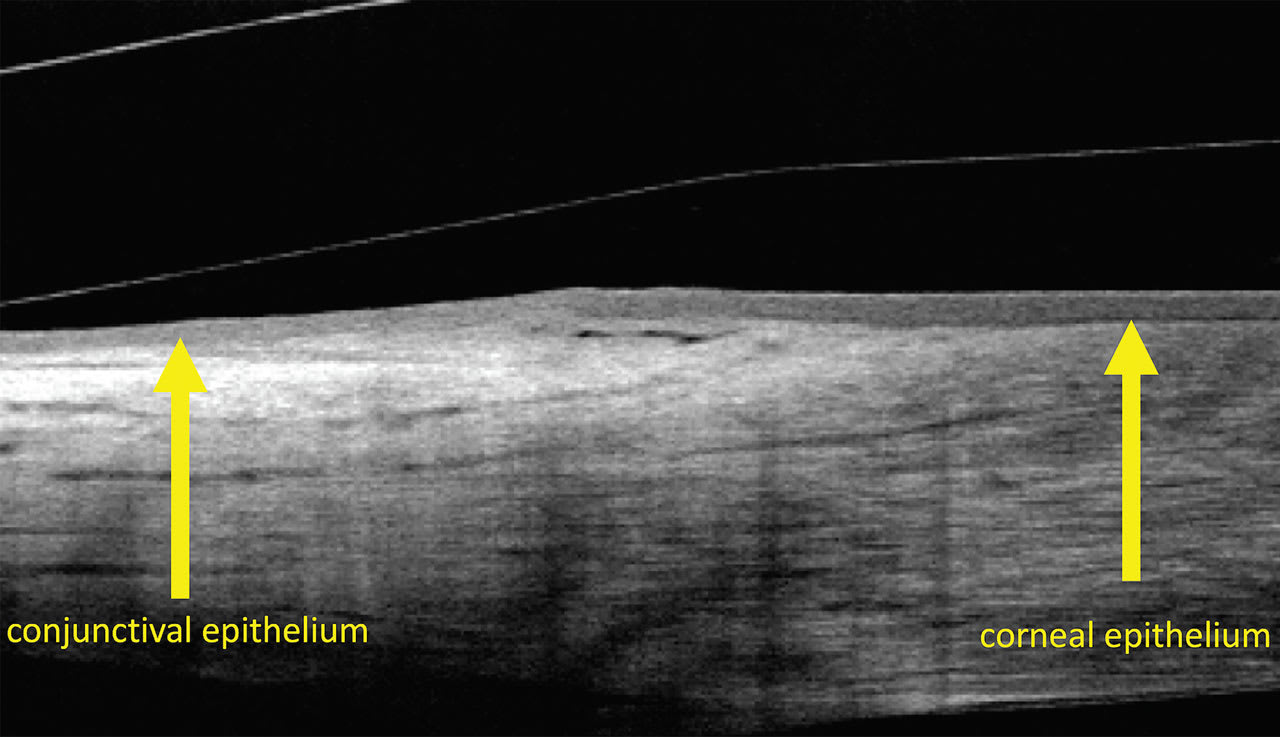
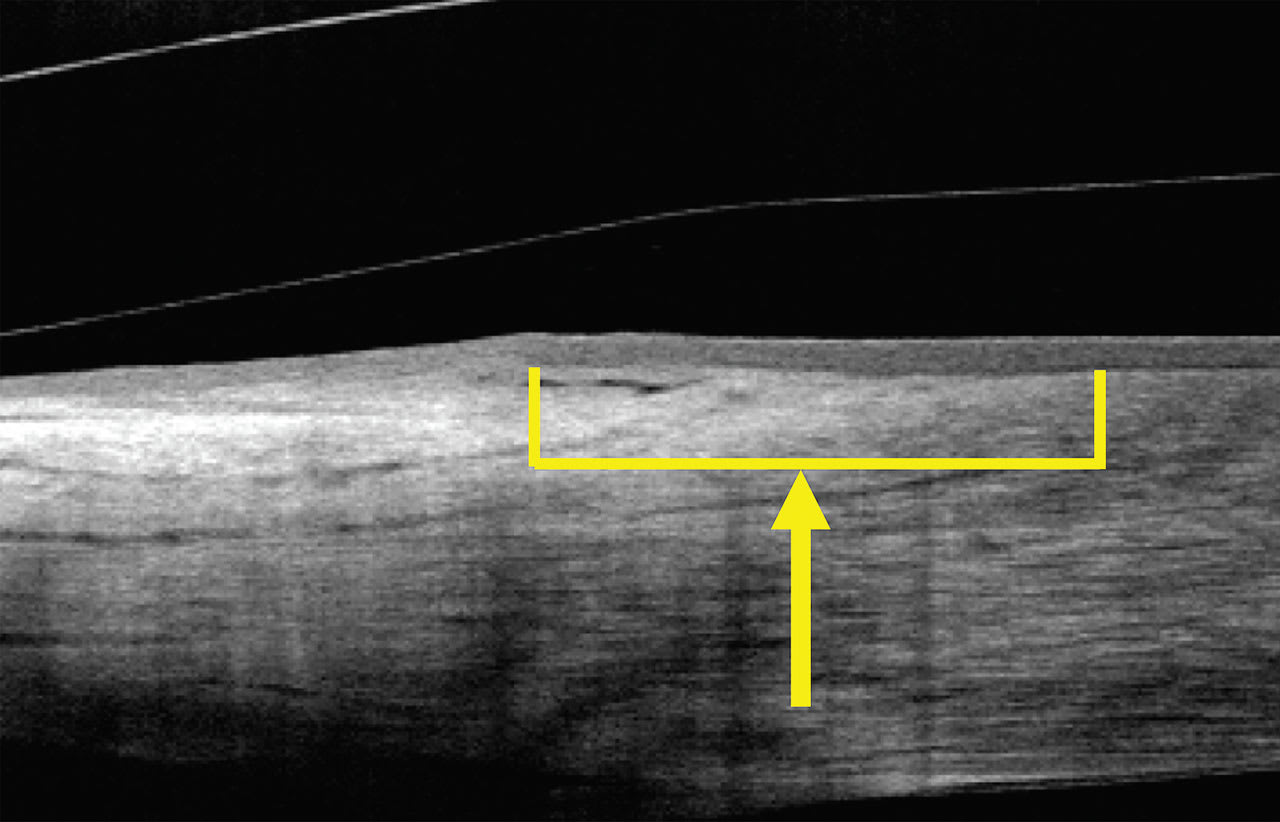
There are other cues that help identify the limbal region. When looking beneath the conjunctival epithelium, the sclera will have a whiter appearance on the OCT scan as this is nontransparent tissue. The cornea, as a transparent tissue, demonstrates a darker appearance.In the region of transition from the sclera to the cornea, the diminishing appearance of the sclera will be observed. Beneath the limbal region of the cornea is a small wedge shape of more hyperfluorescent tissue that helps guide identification of the limbal region (Figure 5). Fortunately, most contemporary lens designs demonstrate a reverse curve between the landing zone and limbal clearance region, which provides the lift necessary for lens elevation and clearance over the limbal region.
LANDING ZONE
The landing zone is critical to align appropriately. It is important to assess the landing zone all the way around the lens. As discussed previously, most scleras have some level of toricity. As such, many clinicians will reach for a diagnostic lens that has a toric landing zone when initially placing it on the eye.
It is critical to determine whether there is toricity to the sclera after lens application. This can be accomplished by rotating the lens on the eye and determining what the lens does after being manually rotated. If the lens rotates back to its original position, it is likely a toric-shaped sclera. If the lens doesn’t rotate back to its original position and remains in the same position as when rotated, it is likely not a toric sclera.
All diagnostic scleral lenses will have markings so the clinician can identify the steep and the flat meridians of the landing zone. Some have markings in the flat meridian, some in the steep meridian, and some in both meridians. When a scleral lens is rotated on the eye, these are the markings to observe to determine whether the lens is prone to consistently rotate to a certain position. Again, if it does, there is scleral toricity present.
If toricity is present, the next step is to determine whether the amount of toricity in the landing zone is the appropriate amount for the sclera. Be sure to assess the lens in both the steep and the flat meridians to determine how much more or less toricity will be required.
This can be easily performed at the slit lamp through visual inspection of the lens in the four major meridians of the landing zone of the diagnostic lens. The fitting characteristics should be similar all the way around the lens. If there is a difference in blood vessel blanching in the different regions of the lens, it usually means that either the lens has a mismatched amount of toricity in the diagnostic lens when compared to the sclera, or the sclera has very little or negligible amounts of toricity. Here are some quick tips that can help assess the lens edge and appropriate adjustments required to the lens.
Impingement This describes additional pressure in a certain part of the landing zone that can lead to blanching of conjunctival blood vessels. If the blanching is at the distal portion of the lens, the toe of the lens is digging into the conjunctiva. This typically means that the toe of the lens needs to be lifted from the surface of the eye in that region of the lens. If the impingement is occurring at the more proximal portion of the landing zone, or the heel of the landing zone, this usually means that either the heel needs to be lifted away from the eye or the toe needs to be brought down closer to the eye.
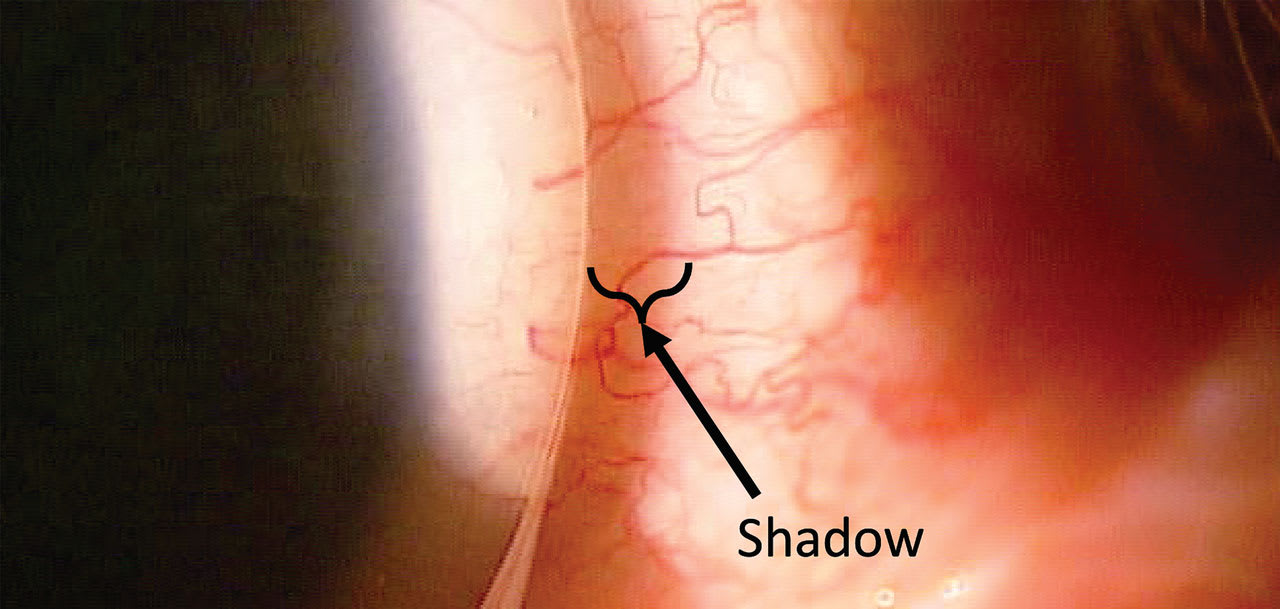
Edge Lift This can sometimes be difficult to observe at the slit lamp. One of the ways that you can more easily see whether edge lift is present is by shining the slit lamp beam on the landing zone and edge of the lens so that the light is projecting on the edge in the direction from the center of the lens to the edge of the lens. This will provide the opportunity for the light to cast a shadow on the conjunctiva past the edge of the lens created by the elevated edge of the lens (Figure 6). The greater the edge lift, the larger the shadow that will be cast on the conjunctival surface.
LEVERAGING OCT FOR THE LANDING
OCT provides vast functionality for both anterior and posterior ocular health assessments. Anterior segment OCT provides the ability to more accurately assess the landing zone and assist in optimizing fit characteristics. However, there are several factors that you need to be cognizant of when assessing landing zone characteristics.
As an example, looking at the cross-section of the most distal portion of the lens on OCT creates a counterintuitive measurement. The OCT is measuring part of the scan through a scleral lens and part that is simply measuring the tissue uncompromised by the plastic of the lens. As such, there will be an image shift at the edge of the lens outside of the region of the lens that will make the conjunctiva and sclera seem elevated. This can make it appear that the edge of the lens is “digging” into the conjunctiva and sclera when in fact in may be appropriately aligned (Figure 7).
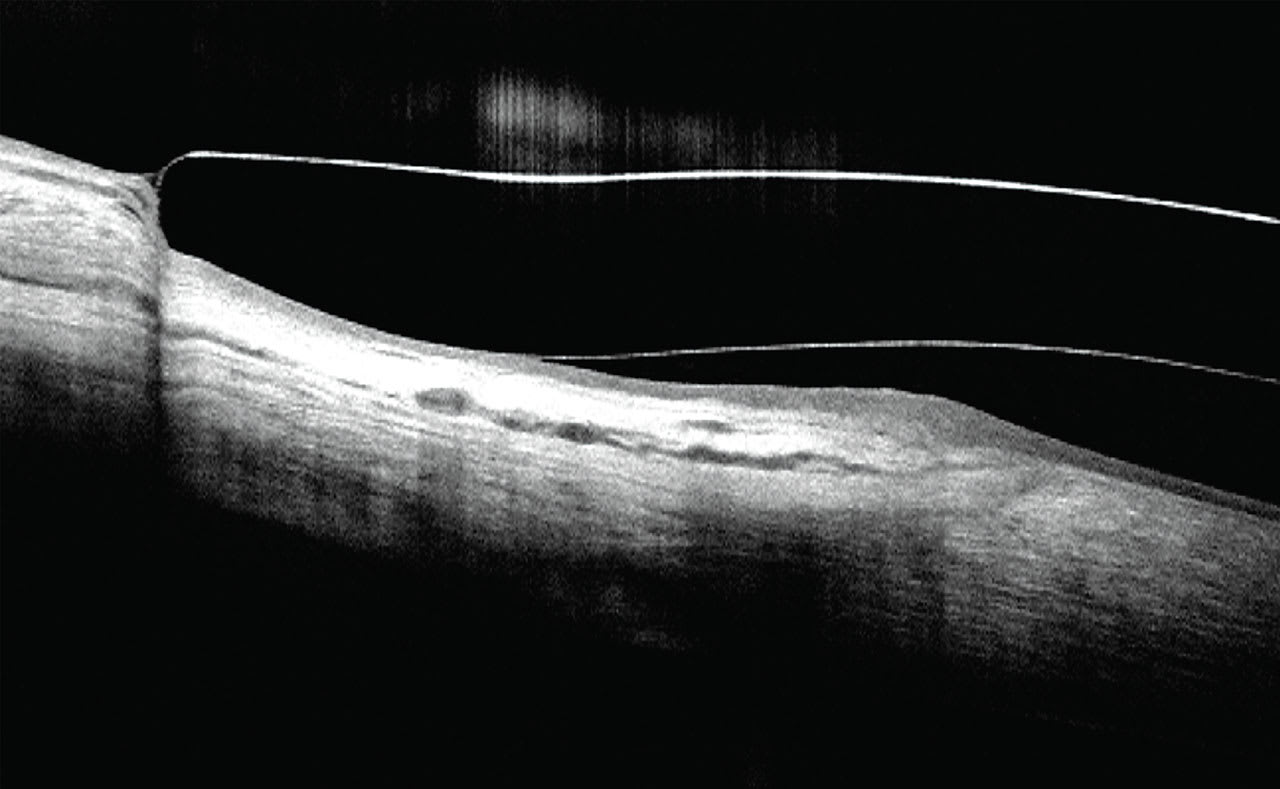
Much of the value with the anterior segment OCT comes from assessing the approach of the landing zone from the proximal region of the landing zone and the trajectory that the landing zone follows as it extends from the proximal region (heel) to the distal region (toe). There should be adequate clearance of the limbal region of the cornea so that the limbus doesn’t have excessive pressure on it. Additionally, the landing zone of the lens should be outside of the region of the limbus.
Following the trajectory of the lens from the heel of the landing zone to the toe, it should maintain a consistent trajectory with the conjunctiva and underlying sclera (Figure 7). If there is a difference between the trajectory of the landing zone and underlying conjunctiva and sclera, it should be adjusted to fit the scleral shape more appropriately.
In instances when there is bearing in the heel region of the landing zone, there can be visible compression of the tissue in that region of the landing zone (Figure 8). Additionally, lens edge lift can also be noted in those patients with a toe-up relationship in the landing zone (Figure 8).
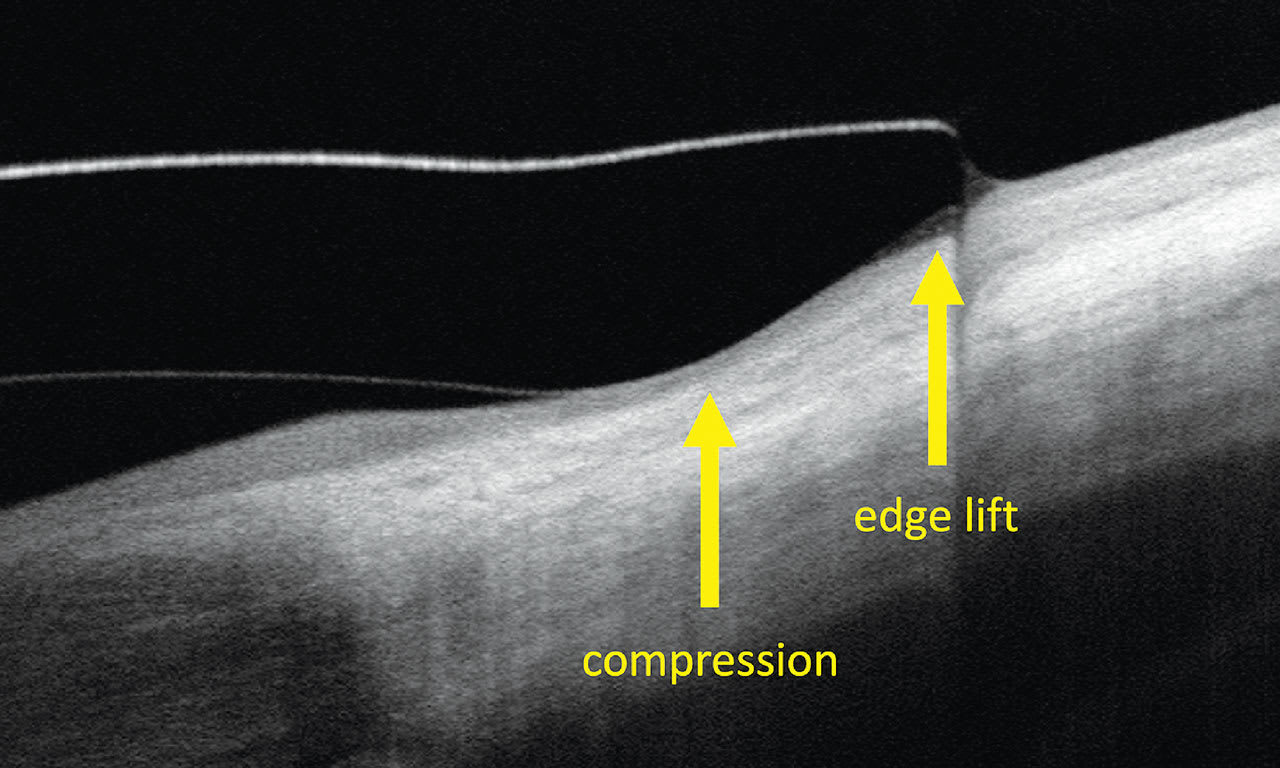
Further, a toe-down fitting relationship can also be observed on an OCT cross section. The trajectory of the landing zone will again not align with the conjunctiva and sclera beneath it. In this situation, there will be bearing in the toe region of the landing zone. Additionally, the heel of the lens can be elevated as well (Figure 9). In this case, either the heel of the landing zone would need to be brought closer to the eye or the toe would need to be elevated to optimize the fit of the lens.

FINAL THOUGHTS
The landing zone is critical to optimizing the blood supply to the limbal region of the cornea and preventing complications with scleral lens wear. Optimizing the fitting relationship with the lens and the landing zone will help improve lens fitting characteristics. Keeping the strategies in mind that were discussed in this article will be sure to optimize scleral fitting success.
REFERENCES
1. DeNaeyer G, Sanders DR, van der Worp E, Jedlicka J, Michaud L, Morrison S. Qualitative Assessment of Scleral Shape Patterns Using A New Wide Field Ocular Surface Elevation Topographer: The SSSG Study. JCLR S. 2017 Nov;1:e12-e22.
2. Nguyen MTB, Thakrar V, Chan CC. EyePrintPRO therapeutic scleral contact lens: indications and outcomes. Can J Ophthalmol. 2018 Feb;53:66-70.
3. EyePrint Prosthetics. Available at eyeprintpro.com. Accessed 2024 Jan 2.
4. Silverman JIM, Huffman JM, Zimmerman MB, Ling JL, Greiner MA. Indications for Wear, Visual Outcomes, and Complications of Custom Imprint 3D Scanned Scleral Contact Lens Use. Cornea. 2021 May 1;40:596-602.
5. Kowalski LP, Collins MJ, Vincent SJ. Scleral lens centration: The influence of centre thickness, scleral topography, and apical clearance. Cont Lens Anterior Eye. 2020 Dec;43:562-567.
6. Addendum. In Phillips AJ, Speedwell L, eds. Contact Lenses (Sixth Edition). Elsevier. 2019:e51-e97.
7. Chen YY, Sun YC, Tsai CY, et al. Spectral-domain optical coherence tomography for evaluating palisades of Vogt in ocular surface disorders with limbal involvement. Sci Rep. 2021 Jun 14;11:12502.
8.Yang Y, Hong J, Deng SX, Xu J. Age-related changes in human corneal epithelial thickness measured with anterior segment optical coherence tomography. Invest Ophthalmol Vis Sci. 2014 Jul 22;55:5032-5038.




