

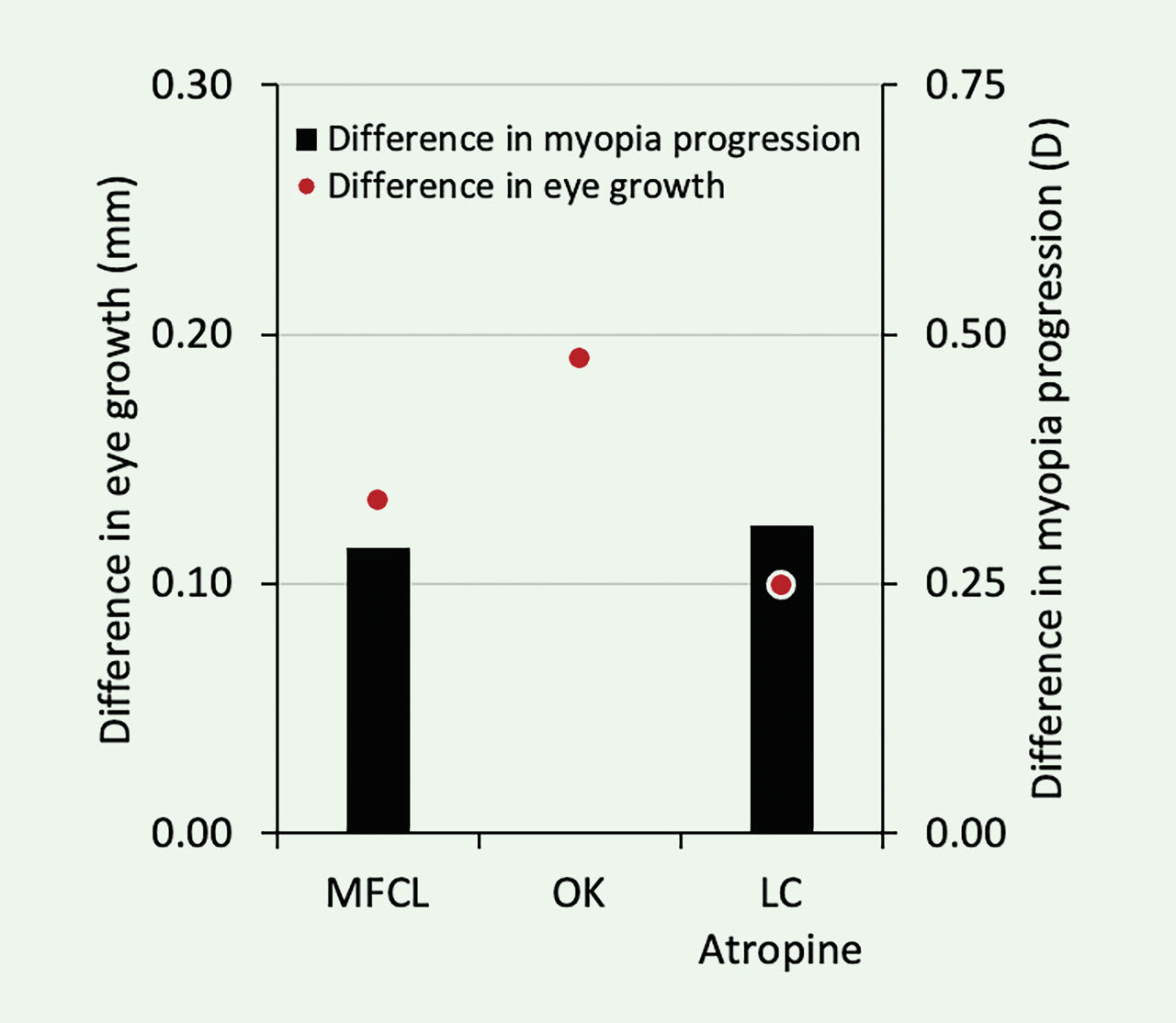
IN THE U.S., eyecare practitioners have a variety of options for myopia control, including soft multifocal1,2 and orthokeratology3 contact lenses, as well as low-concentration atropine.4 While all of these options are effective (Figure 1), providing only one form of myopia control may not provide all patients with the most appropriate or best treatment option. The following article provides eight simple cases with two alternatives for myopia control. This exercise shows that patients have more than one option for myopia control, and each treatment option is optimal for more than one patient. When prescribing myopia control for young children, practitioners should provide a variety of options to the patient and prescribe the one(s) that are likely to provide the best safety and compliance and, therefore, the best likelihood for success.
CASE 1: A 6-YEAR-OLD WHO HAS –7.00D OD AND OS AND WHO DOESN’T HAVE STRONG FINANCIAL MEANS
Soft Multifocal While myopia control options tend to have expensive out-of-pocket costs, there are a few less expensive options. Soft center-distance multifocal contact lenses are an effective form of myopia control,1 while often being less expensive relative to orthokeratology and low-concentration atropine.
Low-concentration atropine requires special formulation from a compounding pharmacy, which adds to the cost of the medication. And, orthokeratology lenses are typically higher priced and may require more time to achieve optimal uncorrected visual acuity for higher myopes, making it is less convenient for the patient; further, orthokeratology is approved by the U.S. Food and Drug Administration (FDA) for up to –6.00D of myopia, while this patient has –7.00D of myopia.
Soft center-distance multifocal lenses are available to not only correct this patient’s refractive error, but rebates may also occasionally be available for these lenses. This can reduce the overall cost for myopia control and makes it a practical myopia control option for this individual.
Atropine Myopia control is being offered at premium prices. As it isn’t covered by insurance, only economically advantaged patients tend to have access to myopia control with the use of atropine. With that in mind, practitioners may consider providing charity eye care to those who cannot afford the care and have a medical necessity for myopia control.
In general, when a patient’s myopia is greater than their age (in this case, the 6-year-old patient has –7.00D myopia), myopia control should be considered medically necessary. An economical form of myopia control may be conducted with occasional dosing of 1% atropine eye drops. A study reported that patients who use 1% atropine one time per month, alternating administration between the eyes every two weeks (place a drop in the right eye on the first day of the month and a drop in the left eye on the 15th day of the month), can reduce myopia progression and eye growth by approximately 75% over two years.5 Although not as commonly prescribed as low-dose atropine, this may be a good option for economically disadvantaged patients who are unable to wear contact lenses, but would still like some myopia control treatment.
CASE 2: AN 11-YEAR-OLD WHO HAS –8.00D OD AND OS
Soft Multifocal Soft center-distance multifocal contact lenses provide patients with the benefits of myopia control while also providing clear vision.1 Additionally, research studies using soft multifocal contact lenses have been successfully completed with younger children with no severe or serious contact lens-related adverse events; therefore, this is generally a safe treatment option for younger children.1 A child who has this high of a myopic prescription would likely be motivated to stay compliant with this modality as their refractive error would be corrected without the use of spectacles.
Currently available center-distance soft multifocals allow for full correction of this patient’s refractive error, and some options extend well beyond this range. Low-concentration atropine alone would not correct this child’s refractive error, while the refractive error may be above the upper limit for successful correction with orthokeratology lenses. This leaves soft center-distance multifocal contact lenses as a preferred modality for myopia control in this case.
Atropine Atropine can provide myopia control while using any type of vision correction, so it is the best option for patients who may be restricted by their prescription or preferences.4 In general, patients who have -8.00D of myopia have fewer treatment options available to them as a result of limitations related to availability or comfort with high prescriptions. For example, high myopes generally require small, round spectacle lenses for the best cosmesis and some contact lenses are not available in the higher myopia range.
A simple eye drop at night can reduce myopia progression and eye growth while allowing a variety of vision correction options during the day. A child could even switch between vision correction modalities as the need or desire fluctuated. As 11-year-old children are extremely active, a variety of options for correction of refractive error provides them with the best opportunity to succeed. Therefore, atropine may be the best myopia control treatment option for a child with high myopia.
CASE 3: A 2-YEAR-OLD WHO HAS –5.00D MYOPIA
Atropine Low-concentration atropine has been found to significantly slow axial elongation while being well tolerated in children.4 While the parent would be administering any method of myopia control at this age, the use of low-concentration atropine with single-vision glasses would provide clear vision while eliminating any potential risk of contact lens complications that may arise from the use of soft multifocal or orthokeratology lenses.
It is worth noting that one study found that younger children using 0.05% atropine displayed a similar reduction of axial elongation as older children using 0.01% atropine.6 In the case of this 2-year-old who has –5.00DS of myopia, a lower concentration of atropine can be attempted initially; however, the concentration may need to be increased to a slightly higher concentration of low-concentration atropine if the desired treatment effect is not obtained on the lowest dose.
Orthokeratology While many people would not want to fit a 2-year-old child with contact lenses, orthokeratology may be a good option for this patient. Orthokeratology contact lenses are worn at night, so a parent is always present during treatment. Parents can perform all of the contact lens care and ensure proper wear and care is achieved.
Fitting a 2-year-old with orthokeratology can also ensure that the child experiences clear vision throughout the day, whereas glasses can be easily removed, resulting in blurry vision. Even for children who are hesitant to have contact lenses applied, orthokeratology provides a nice option as the contact lenses can be applied after the child falls asleep. Amazingly, some children may not even wake up upon application of the contact lenses.
Orthokeratology is, therefore, a treatment option that is controlled completely by the parent, provides clear vision throughout the day, and has been shown to slow eye growth, even in high myopes.7
CASE 4: A 9-YEAR-OLD WHO HAS A REFRACTION OF –3.00 –2.50 X 180 OD AND OS
Orthokeratology When considering orthokeratology as a method of myopia control for a myope with moderate corneal astigmatism, it is necessary to know whether the astigmatism is central or limbus-to-limbus as shown on corneal topography. While spherical orthokeratology designs can often be used for with-the-rule astigmatism up to 1.75DC, a design utilizing toric reverse or alignment curves should be considered when moderate limbus-to-limbus astigmatism is present to achieve an optimal centration.
This becomes especially important for myopia control, as a decentered lens may not lead to as significant of a myopia control effect as a centered lens would.8 One study found that in cases of moderate-to-high corneal astigmatism, utilizing a toric orthokeratology design resulted in improved lens centration and slower axial elongation,8 showing that orthokeratology could still be a viable method of myopia control for this 9-year-old with 2.50DC.
Soft Multifocal In the not-too-distant past, there were few myopia control options available for children who have astigmatism. Today, there are several options available. Toric multifocal contact lenses, especially toric multifocal contact lenses in center-distance design, are difficult to find. However, there is at least one option available. This lens provides myopia control with stable astigmatism correction for a wide range of cylinder powers and axes, making it an excellent myopia control treatment option for children with high astigmatism.
Soft multifocal contact lenses used for myopia control should have a center-distance design and incorporate the highest add power.1 Soft contact lenses require little time for adaptation, provide consistently clear vision, and improve children’s self-perceptions.9 Soft contact lenses are also advantageous when corneal toricity does not match the refractive astigmatism.
CASE 5: A 6-YEAR-OLD WHO HAS –4.50D OD AND OS, AND 12∆ ACCOMMODATIVE ESOPHORIA
Soft Multifocal The treatment for a child symptomatic with accommodative esophoria at near would be an add power to reduce the accommodative demand, which in the case of a high accommodative convergence that occurs per diopter of accommodative response (AC/A) ratio will reduce the esophoric posture at near. When considering myopia control options that could additionally help the near esophoria as well, center-distance soft multifocal contact lenses would be a suitable option. If children utilize the add power of the multifocal contact lens, their accommodation may relax leading to a more exophoric posture.
While more research is needed in this area, a study found that children wearing center-distance multifocal contact lenses may exhibit a more exophoric posture at near with a reduced accommodative response.10 This treatment modality could then provide the benefits of clear distance vision, myopia control, and the potential of reducing symptoms of near esophoria.
Orthokeratology The putative cue for contact lens myopia control is myopic defocus. While myopic defocus is created by the peripheral part of the contact lens, the myopic defocus is actually presented to the entire retina. In fact, that is how presbyopic contact lens designs provide clear near vision for adults over 40 years of age. In orthokeratology, the mid-peripheral cornea is steepened, resulting in peripheral defocus that theoretically slows myopia progression and provides a reading add that can reduce accommodation.
Children with accommodative esophoria generally have very high AC/A ratios, so a small reduction in accommodation can dramatically reduce near-point esophoria. As the amount of peripheral myopic defocus is related to the amount of baseline myopia for orthokeratology contact lens wearers,11,12 children who have high-to-moderate baseline myopia can expect a less esophoric posture when fit with orthokeratology contact lenses. Therefore, fitting a young myopic patient with orthokeratology can solve many issues including reducing myopic eye growth, reducing near-point esophoria, and allowing clear vision throughout the day without vision correction.
CASE 6: AN 11-YEAR-OLD COMPETITIVE SWIMMER WHO HAS –4.00D OD AND OS
Orthokeratology Research shows that swimming in contact lenses is a risk factor for developing Acanthamoeba keratitis (an infection caused by a pathogen that can be found in a variety of water sources).13 Therefore, when considering myopia control options for a competitive swimmer, it is vital to choose an option that does not increase the risk of infection.
As orthokeratology lenses are worn at night, this modality would provide the benefits of myopia control as well as clear vision during the day and allow for swimming without the need for wearing contact lenses while in or around the water. While prescription goggles are a viable alternate form of vision correction that can be used during swimming, orthokeratology would provide clear vision even when the individual is outside of the pool without goggles on.
Atropine Contact lenses have been shown to accumulate microbial organisms during wear in a swimming pool,14 and this may increase the risk of microbial keratitis. As competitive swimmers spend so much time in the pool, atropine eye drops are a great option for myopia control. Today, swimming goggles are available with prescription lenses, thus providing competitive swimmers with clear vision during competitions in the pool. Even swimmers who don’t require vision correction wear goggles in the pool; so goggles don’t negatively affect the performance of young, competitive swimmers. Slowing the progression of myopia is possible with nightly administration of low-concentration atropine eye drops, so the patient can go about their day as normal without increasing the risk of a potentially sight-threatening complication such as microbial keratitis.
CASE 7: A 6-YEAR-OLD PATIENT WHO HAS +0.25D OD AND OS
Atropine For every year younger the onset of myopia, patients are expected to be –0.86D more myopic and almost three times more likely to be a high myope as adults.15 Therefore, delaying the onset of nearsightedness not only allows children additional time with correction-free clear vision, it may also result in lower myopia in adulthood and, therefore, lower risk of sight-threatening complications.16
Studies have shown low-concentration atropine to be effective in delaying the onset of myopia in children who are pre-myopic.17-19 As pre-myopes would not notice any vision benefits from other forms of myopia management, such as center-distance multifocal contact lenses or orthokeratology, low-concentration atropine is a suitable option to optimize compliance and, therefore, the intended treatment effect. While outdoor time may vary seasonally, low-concentration atropine can be administered year-round. Further, parents may administer the eye drops to ensure that the benefits are uninterrupted and regulated.
Outdoor Time Two options have been shown to effectively delay the onset of myopia: low-concentration atropine19 and increased outdoor time20 (Table 1). Atropine requires parents to administer eye drops nightly to young children who generally dislike having anything instilled in their eyes. Atropine is also an antimuscarinic agent that potentially leads to photophobia and cycloplegia.
Conversely, increasing outdoor time can delay myopia progression while providing other benefits such as increased activity21 and vitamin D.22 For those concerned about increasing exposure to ultraviolet light by increasing outdoor time, sunglasses protect the eyes while allowing higher doses of light than indoors and greater than threshold illuminance for myopia prevention.23 Therefore, outdoor time is another suitable option for delaying the onset of myopia.
CASE 8: AN 8-YEAR-OLD WHO HAS –2.25D OD AND OS WITH POOR HYGIENE HABITS
Atropine For patients who have poor hygiene habits, low-concentration atropine is an appropriate myopia control method, as it is effective4 and allows treatment to occur while at home under the supervision of a parent to ensure proper hygiene during eye drop instillation. This child could then wear glasses to correct their refractive error, as contact lenses may be a suboptimal option due to the child’s poor hygiene habits.
Poor contact lens care and hygiene habits, such as sleeping in contact lenses, exposing contact lenses to water, or poor hand hygiene, can increase a contact lens wearer’s risk of developing microbial keratitis, which can have a lasting impact on the eyes and vision.26 Low-concentration atropine provides a safe modality for myopia control and ensures that no contact lens-related adverse events occur.
Orthokeratology Poor hygiene habits may lead to greater risk of sight-threatening complications, such as microbial keratitis.27 Patients who have poor hygiene habits are often discouraged from wearing contact lenses for this reason. However, orthokeratology contact lenses may be a suitable option for this patient as the child only wears the contact lenses while under the supervision of a parent or during sleep.
Parents can play a more active role in the care of orthokeratology contact lenses as they are worn only at home and during the night. If necessary, the parent can supervise the care regimen to make sure that appropriate cleaning occurs prior to handling of the contact lenses and upon removal. The lenses are never worn during the day, when disruption to wear can lead to mishandling of the contact lenses and poor hygiene that puts the patient at risk. The orthokeratologic effect also ensures clear vision throughout the school day, potentially improving the child’s academic performance.
REFERENCES
1. Walline JJ, Walker MK, Mutti DO, et al; BLINK Study Group. Effect of High Add Power, Medium Add Power, or Single-Vision Contact Lenses on Myopia Progression in Children: The Blink Randomized Clinical Trial. JAMA. 2020 Aug 11;324:571-580.
2. Chamberlain P, Peixoto-de-Matos SC, Logan NS, Ngo C, Jones D, Yougn G. A 3-Year Randomized Clinical Trial of Misight Lenses for Myopia Control. Optom Vis Sci. 2019 Aug;96:556-567.
3. Cho P, Cheung SW. Retardation of Myopia in Orthokeratology (Romio) Study: A 2-Year Randomized Clinical Trial. Invest Ophthalmol Vis Sci. 2012 Oct 11;53:7077-7085.
4. Yam JC, Jiang Y, Tang SM, et al. Low-Concentration Atropine for Myopia Progression (Lamp) Study: A Randomized, Double-Blinded, Placebo-Controlled Trial of 0.05%, 0.025%, and 0.01% Atropine Eye Drops in Myopia Control. Ophthalmology. 2019 Jan;126:113-124.
5. Zhu Q, Tang Y, Guo L, et al. Efficacy and Safety of 1% Atropine on Retardation of Moderate Myopia Progression in Chinese School Children. Int J Med Sci. 2020 Jan 1;17:176-181.
6. Li FF, Zhang Y, Zhang X, et al. Age Effect on Treatment Responses to 0.05%, 0.025%, and 0.01% Atropine: Low-Concentration Atropine for Myopia Progression Study. Ophthalmology. 2021 Aug;128:1180-1187.
7. Charm J, Cho P. High Myopia-Partial Reduction Ortho-K: A 2-Year Randomized Study. Optom Vis Sci. 2013 Jun;90:530-539.
8. Zhang Y, Chen YG. Comparison of Myopia Control between Toric and Spherical Periphery Design Orthokeratology in Myopic Children with Moderate-to-High Corneal Astigmatism. Int J Ophthalmol. 2018 Apr 18;11:650-655.
9. Walline JJ, Jones LA, Sinnott L, et al. Randomized Trial of the Effect of Contact Lens Wear on Self-Perception in Children. Optom Vis Sci. 2009 Mar;86:222-232.
10. Gong CR, Troilo D, Richdale K. Accommodation and Phoria in Children Wearing Multifocal Contact Lenses. Optom Vis Sci. 2017 Mar;94:353-360.
11. Charman WN, Mountford J, Atchison DA, Markwell EL. Peripheral Refraction in Orthokeratology Patients. Optom Vis Sci. 2006 Sep;83:641-648.
12. Kang P, Swarbrick H. Peripheral Refraction in Myopic Children Wearing Orthokeratology and Gas-Permeable Lenses. Optom Vis Sci. 2011 Apr;88:476-482.
13. Radford CF, Minassian DC, Dart JK. Acanthamoeba Keratitis in England and Wales: Incidence, Outcome, and Risk Factors. Br J Ophthalmol. 2002 May;86:536-542.
14. Choo J, Vuu K, Bergenske P, Burnham K, Smythe J, Caroline P. Bacterial Populations on Silicone Hydrogel and Hydrogel Contact Lenses after Swimming in a Chlorinated Pool. Optom Vis Sci. 2005 Feb;82:134-137.
15. Chua SY, Sabanayagam C, Cheung YB, et al. Age of Onset of Myopia Predicts Risk of High Myopia in Later Childhood in Myopic Singapore Children. Ophthalmic Physiol Opt. 2016 Jul;36:388-394.
16. Bullimore MA, Brennan NA. Myopia Control: Why Each Diopter Matters. Optom Vis Sci. 2019 Jun;96:463-465.
17. Fang PC, Chung MY, Yu HJ, Wu PC. Prevention of Myopia Onset with 0.025% Atropine in Premyopic Children. J Ocul Pharmacol Ther. 2010 Aug;26:341-345.
18. Jethani J. Efficacy of low-concentration atropine (0.01%) eye drops for prevention of axial myopic progression in premyopes. Indian J Ophthalmol. 2022 Jan;70:238-240.
19. Yam JC, Zhang XJ, Zhang Y, et al. Effect of Low-Concentration Atropine Eyedrops Vs Placebo on Myopia Incidence in Children: The Lamp2 Randomized Clinical Trial. JAMA. 2023 Feb 14;329:472-481.
20. He M, Xiang F, Zeng Y, et al. Effect of Time Spent Outdoors at School on the Development of Myopia among Children in China: A Randomized Clinical Trial. JAMA. 2015 Sep 15;314:1142-1148.
21. Burdette HL, Whitaker RC, Daniels SR. Parental Report of Outdoor Playtime as a Measure of Physical Activity in Preschool-Aged Children. Arch Pediatr Adolesc Med. 2004 Apr;158:353-357.
22. Müller DN, Kleinewietfeld M, Kvakan H. Vitamin D Review. J Renin Angiotensin Aldosterone Syst. 2011 Jun;12:125-128.
23. Lanca C, Teo A, Vivagandan A, et al. The Effects of Different Outdoor Environments, Sunglasses and Hats on Light Levels: Implications for Myopia Prevention. Transl Vis Sci Technol. 2019 Jul 18;8:7.
24. Wu PC, Tsai CL, Wu HL, et al. Outdoor Activity During Class Recess Reduces Myopia Onset and Progression in School Children. Ophthalmology. 2013 May;120:1080-1085.
25. Jin JX, Hua WJ, Jiang X, et al. Effect of Outdoor Activity on Myopia Onset and Progression in School-Aged Children in Northeast China: The Sujiatun Eye Care Study. BMC Ophthalmol. 2015m Jul 9;15:73.
26. Lim CH, Carnt NA, Farook M, et al. Risk Factors for Contact Lens-Related Microbial Keratitis in Singapore. Eye (Lond). 2016 Mar;30:447-455.
27. Wagner H, Richdale K, Mitchell GL, et al. Age, Behavior, Environment, and Health Factors in the Soft Contact Lens Risk Survey. Optom Vis Sci. 2014 Mar;91:252-261.




