LEARNING METHOD AND MEDIUM
This educational activity consists of a written article and 20 study questions. The participant should, in order, read the Activity Description listed at the beginning of this activity, read the material, answer all questions in the post test, and complete the Activity Evaluation/Credit Request form. To receive credit for this activity, please follow the instructions provided below in the section titled To Obtain CE Credit. This educational activity should take
a maximum of two hours to complete.
CONTENT SOURCE
This continuing education (CE) activity captures key statistics and insights from contributing faculty.
ACTIVITY DESCRIPTION
In this article, the authors explore what we know about current methods of soft lens fitting and its limitations. It focuses on the back surface shape in relation to the ocular shape and the front surface optical profiles (for myopia management).
TARGET AUDIENCE
This educational activity is intended for optometrists, contact lens specialists, and other eyecare professionals.
ACCREDITATION DESIGNATION STATEMENT
This course is COPE accredited for two hours of CE credit.
COPE Course ID: 93800-CL
COPE Activity ID: 129541
DISCLOSURES
Eef van der Worp, PhD, has received education grants from Contamac Ltd., Johnson & Johnson Benelux, and Bausch + Lomb Boston Materials. Mari Fujimoto, OD, reports no conflicts of interest. Patrick J. Caroline reports no conflicts of interest.
DISCLOSURE ATTESTATION
The contributing faculty member has attested to the following:
1. That the relationships/affiliations noted will not bias or otherwise influence their involvement in this activity;
2. That practice recommendations given relevant to the companies with whom they have relationships/affiliations will be supported by the best available evidence or, absent evidence, will be consistent with generally accepted medical practice;
3. That all reasonable clinical alternatives will be discussed when making practice recommendations.
TO OBTAIN CE CREDIT
To obtain COPE CE credit for this activity, read the material in its entirety and consult referenced sources as necessary. We offer instant certificate processing for COPE credit. Please take the post test and evaluation online by using your OE tracker number and logging in to visioncarece.com.
Upon passing the test, you will immediately receive a printable PDF version of your course certificate for COPE credit. On the last day of the month, all course results will be forwarded to ARBO with your OE tracker number, and your records will be updated. You must score 70% or higher to receive credit for this activity. Please make sure that you take the online post test and evaluation on a device that
has printing capabilities.
NO-FEE CONTINUING EDUCATION
There are no fees for participating in and receiving credit for this CE activity.
Disclaimer
The views and opinions expressed in this educational activity are those of the faculty and do not necessarily represent the views of Contact Lens Spectrum. This activity is copyrighted to BroadcastMed LLC ©2024. All rights reserved.
CE Questions? Contact eventhelp@broadcastmed.com for help.
Release Date: November 1, 2024
Expiration Date: October 7, 2027



THE PRIME TASK AND GOAL when fitting contact lenses is to “first, do no harm,” ensuring that corneal integrity is compromised as little as possible by the lens shape, with no visible mechanical signs of lens wear and as little impact as possible on comfort of wear.
In rigid corneal and scleral lens fits, this is an obvious necessity that requires a high level of accuracy. In soft lens fitting, there certainly is more leeway, but that does not mean “shape” can be ignored altogether. Does one size fit all? This article explains why one size fits some—or, more accurately, most—but not all. Surprisingly, there is not much evidence to support base curve (BC)-based soft lens fitting in practice. So, the question is: Can we do better with soft lens fitting?
All this becomes increasingly important if we want to fit potentially millions of kids into soft lenses for myopia management purposes. Additionally, while we have an impressive number of soft lens wearers, the rate of people dropping out of lens wear is also substantial. According to Pucker and Tichenor, the pooled dropout frequency, based on a combination of several studies with a total of 8,190 subjects, is estimated to be 21.7%.1 If the goal is to impact the corneal integrity as little as possible, with no visible mechanical signs of lens wear and minimal impact on comfort of wear, it is important to look more closely at the soft lens fitting process.
THE STARTING POINT
First and foremost, it is crucial to determine the health status of the eye and the ocular surface. There are better lenses now than ever before, but standard lenses are designed for normal eyes. Looking at factors such as the central keratometry values, corneal diameter, and eccentricity separately is not sufficient to determine eye shape, but the combination of these factors can be summarized as the sagittal height (SAG) value and provides practitioners with a good starting point.
Developments in the last decade or so have been instrumental, literally, in imaging a larger portion of the ocular surface beyond just the cornea. Corneal topographers have been available for quite some time now, but they typically measure only a small portion of the ocular surface. Modern technology such as optical coherence tomography (OCT), profilometry, and Scheimpflug imaging have given practitioners much more insight into the ocular surface shape over a larger diameter.
Corneal topographers can now estimate the sagittal height values of the ocular surface (OC-SAG). Figure 1 shows an overview of different studies looking into the average OC-SAG over a 15mm chord measured with several different commercial systems or estimated height calculation by a corneal topographer.2-14 A normal eye over that area would have an OC-SAG of around 3,720 microns on average based on these studies, with a standard deviation of 175 microns. This means that most eyes would be approximately 3,550 to 3,900 microns in height, which would represent 68% of “normal” eyes, but there is some variation based on the instrument used.
One factor we need to consider in discussing this method further is that OC-SAG values vary in different meridians. Rojas and colleagues recently showed that if we only measure the horizontal OC-SAG, the absolute differences with the vertical meridian over a 15mm chord with profilometry and with OCT are respectively 103 ± 92 microns and 109 ± 79 microns—and this difference can be up to 200 microns (maximum) between any two meridians.12 This means there is a small “error” when measuring one meridian alone, and ideally it would be better to measure the ocular surface in a 360° manner.
The 15mm chord traditionally has been chosen because soft lenses are typically 14.2mm to 14.5mm in diameter and move about 0.2mm to 0.3mm on each side. For future research, it may be better to use the size of the actual lens to be fitted as a reference to match the CL-SAGs directly, but many more questions must be answered before we can support this.
UP OUR GAME
The next area to evaluate is the back surface shape of the lens: What is being fitted on the eye? Traditionally, as inherited from corneal rigid lenses, soft lens nomenclature has included BC as a primary parameter. Most eyecare professionals (ECPs) regard BC as the leading factor in soft lens fitting. Several studies have shown, however, that there is very little correlation between BC and soft lens behavior on the eye.16-17
Additionally, studies have shown that lenses from two different companies with a BC of, for example, 8.6mm can have SAG values that vary quite dramatically (more than 400 microns).18 All BC really tells practitioners is that a lens with a BC of 8.7mm is “flatter” than one with a BC of 8.3mm—but only if the lenses are of the same type/material and diameter. On average, lens designs that are offered in two BCs differ by about 275 microns in SAG.18
Interestingly—and confusingly—there is no set rule to define the BC value on the package; some companies calculate the “BC equivalent” based on the overall average BC over the full lens diameter. Others arbitrarily use, for example, a 10mm chord. This may explain why BC values often don’t make sense.
Soft lens parameters may need to be redefined as deep and shallow in terms of sagittal depth, rather than steep and flat in terms of radius. And “microns of height” may become the new “millimeters of curvature,” if we want to up our game of soft lens fitting in terms of height.
GOING IN DEPTH ON SAGITTAL DEPTH
Several studies have looked at soft lens shape,18-20 all measuring lenses in saline at 20° Celsius by International Organization for Standardization (ISO) standards.21 What these studies showed is that there is a wide variety of lens SAGs (CL-SAGs), but it is not unlimited; the major companies cater to the top of the bell curve of normal eyes.
It is obvious, however, that these standard lenses cannot work for every eye; eyes that are quite flat or steep in nature (or, in the new terminology, have a low or high SAG value) could benefit from a lower or higher CL-SAG value. This may be best achieved by considering lenses that are situated respectively on the left or right side of the graph (Figure 2) or by switching to an individually designed lens. This will give ECPs, at minimum, some confidence in the process of soft lens fitting, which the profession has lost to some degree.
A study by Dutta and colleagues investigated the relationship between CL-SAG and OC-SAG with regard to lens fit and subjective comfort.11 Participants who have high, median, and low OC-SAGs were recruited and fitted with three lenses with different CL-SAG values.
Fitting low- or high-CL-SAG lenses on high- or low-OC-SAG eyes, respectively, led to suboptimal movement and eventually to a tighter fit after several hours. In short, CL-SAG values can be clinically relevant in soft lens fitting on out-of-standard eyes to optimize lens fit and comfort.
What is known from studies is that a soft lens needs to be somewhat “deeper” than the ocular surface to achieve a successful fit.9,22 Simply put, a soft lens needs “grip”; otherwise, the lens moves excessively under the influence of eyelid pressure, tear film variables, lubrication, etc., and can be uncomfortable. How much higher in SAG a lens should be is the clinical question that we need to answer, but it is still quite a puzzle.
One part of that puzzle may be the temperature at which the lenses are measured. The temperature of the ocular surface is estimated to be 34° Celsius, and not the ISO standard of 20° Celsius. A recent study shows that all soft lenses shrink by an average of 3% when going from room temperature to eye temperature, but there are substantial differences among lens materials.20 Typically, lenses with higher water content shrink more.20 In some lenses, the difference exceeds 5%.
It was not the goal of this study to single out lenses or judge their performance. But it could be argued that, at least from a theoretical standpoint, using the 34° Celsius values (eye temperature) in the future would make more sense than using room temperature values (Figure 2).
CORNEAL INFILTRATIVE EVENTS
A recent study presented at the 2024 the Association for Research in Vision and Ophthalmology (ARVO) meeting showed that lenses that do not match the ocular surface shape can result in a higher rate of corneal infiltrative events (CIEs) or microbial keratitis (MK).23 Andrew and co-workers23 looked at 25 contact lens wearers who had these events documented within the last two years and correlated this with corneal sagittal height at a 12mm chord calculated from topography.
Contact lens wearers with adverse events had a corneal sagittal height that was significantly shallower compared to the population mean. It was concluded that one-size-fits-most soft contact lenses may have a CL-SAG that is too deep for patients who have a shallower-than-typical corneal sagittal depth, which could increase adverse event risk.
AN ELEPHANT IN THE ROOM
There is an elephant in the room when it comes to educating students and ECPs about soft lens fitting. To them, the way it has traditionally been performed “doesn’t make sense”; and to be frank, they are right—using BCs doesn’t make sense. Unfortunately, lens movement is not a good metric to assess whether we have the right lens on the eye. Sometimes lenses decenter because they are too flat (or shallow); they decenter slightly and then appear “stuck” or limited in movement.
In other cases, the difference between two BCs (even using the same lens type and manufacturer) does not appear to result in any difference in movement. Even if measured digitally in decimals of accuracy, differences in lens movement are often hardly detectible. This was confirmed in another recent study: CL-SAG was not significantly correlated with post-blink lens movement in primary gaze or upgaze, and the push-up recovery time was not significantly correlated either.24 While clinicians can use fluorescein patterns to assess relative sagittal depth for rigid corneal and scleral lenses, the assessment technique used in soft lens fitting may not be very reliable.
OPTICS, PRESBYOPIA, AND MYOPIA
Then there are the optics of the lenses, which haven’t been discussed yet. Coming back to the topic of dropouts, studies have shown clearly that vision and comfort are highly correlated.1 In other words, patients who don’t see well experience more discomfort. This association was clear, especially in the neophyte and presbyopia dropout groups.
Another study found that patients with presbyopia who drop out of contact lenses have a corneal sagittal depth that is further from the population mean than that of the average wearers.25 This indicates that the CL-SAGs of lenses may have been either too shallow or too steep for these patients’ eyes and may have contributed to lens decentration, visual discomfort, and contact lens dropout. The study’s recommendation is that clinicians should assess corneal shape in patients who are not successful in presbyopic contact lenses and consider a custom design instead of a standard design.
Going from the back surface to the front surface of the lens, Plainis and Charman showed that “flexing” of a soft lens on the ocular surface can influence the dioptric value.26 These values were small and may not be all that relevant clinically, especially in the lower power ranges. However, for more complex lens optics—including multifocal lenses, lenses for myopia management, and lenses with higher-order aberration correction—this could be an issue. Having control over the amount of flexing (the amount of SAG difference between the lens and the eye) might be valuable in predicting the optical change. More recently, Abass and co-workers also found an impact in effective optical power change of soft contact lenses with high ametropic values after placing lenses on the eyes.27
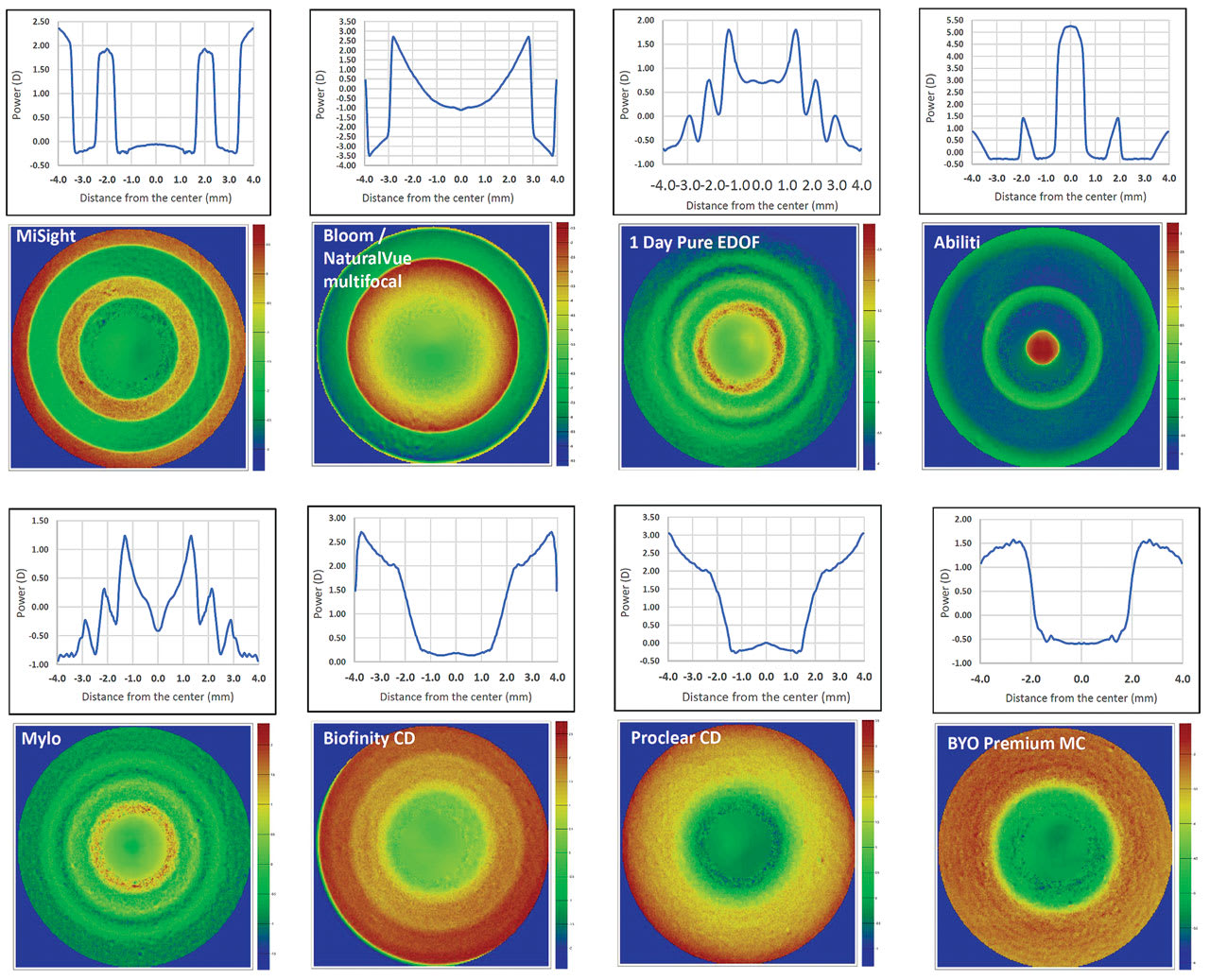
Power profiles and design of soft lenses used for myopia management were recently published28 (see Figure 3). Looking at different on- and off-label lenses for myopia management, two primary observations were apparent.
First, different optical profiles can induce different optical effects on the eye. ECPs may choose one of the four defined principal categories (multiconcentric, multifocal, extended depth of focus [EDOF], and torus) over the others when changing the lens design. If a lens in a certain category does not provide satisfactory myopia management results, switching to another category makes more sense in theory compared to trying another lens in the same category, but this certainly merits more investigation.
Second, there are significant differences in SAG values among myopia management lenses.28 This can induce a different lens fit and impact lens centration as well as the myopia management outcomes. The differences in CL-SAG are not necessarily reflected by BC values. As an illustration, a new myopia management soft lens on the market has a listed BC of 7.9mm but is “middle of the road” in terms of the CL-SAGs of soft lenses for myopia management.
As scleral lenses decenter slightly temporally, due to differences in nasal versus temporal anterior scleral shape characteristics,29 soft lenses do too. But soft lenses that are too shallow for the eye decenter more. This may not impact the optics of single-vision lenses, but with multifocal and myopia management lenses, it can have a significant impact. Thus, lens fit and lens optics are highly correlated and should be evaluated together for an optimal result. Typically, if the CL-SAG is deeper, then temporal decentration can be reduced.
CLOSING REMARKS
One take-home message is that BCs are arbitrary values when fitting soft lenses. In addition, selecting a CL-SAG value (probably best at 34° Celsius) to better match a shallow or deep ocular sagittal height may offer a more efficient method of fitting soft lenses compared to relying solely on the lens base curve. OC-SAG, which can be measured or at least estimated by currently available instruments in clinical practice, is a key starting point. The next step is to understand soft lens behavior on eye, and practitioners may need other evaluation techniques for soft lenses on eye than lens movement.
While there is still much to learn and to explore in soft lens fitting, one factor seems clear: When an eye has a low sagittal height value (flat eye), it does not make sense to use a high or even a medium CL-SAG lens from the right side of the graph. Selecting a lens from the left side makes more sense in that case, without taking the absolute numbers and sometimes small differences between lenses too seriously. If a standard lens is not sufficient, a custom-made lens may help improve performance and reduce dropouts. Of course, the reverse is also true — deep eyes should not be fit with shallow lenses.
But SAG does not tell the whole story or solve all our problems. The variation in CL-SAG of standard lenses for normal eyes is not all that great, and other lens variables—such as material properties, design, edge design, and lens dehydration during the day—may play as crucial a role (or bigger) in lens comfort and success. But one might start by looking at ocular surface shape and combine that with the awareness of the shapes of the lenses on the market. That could make a great beginning.
In short, we are learning more and more about soft lens fitting and soft lens behavior on eye, but it is a relatively steep learning curve. “Deep” may be a more appropriate term, as it may be time to move away from using BC values to give ECPs better tools to fit soft lenses.
REFERENCES
1. Pucker AD, Tichenor AA. A Review of Contact Lens Dropout. Clin Optom (Auckl). 2020 Jun 25;12:85-94.
2. Sorbara L, Maram J, Fonn D, Woods C, Simpson T. Metrics of the normal cornea: anterior segment imaging with the Visante OCT. Clin Exp Optom. 2010 May;93:150-156.
3. Achong-Coan R, Caroline PJ, Kinoshita B, et al. How do normal and keratoconic eyes differ in shape? Poster presented at the 2012 Global Specialty Lens Symposium, Las Vegas. 2012 Jan 26-29.
4. Hall LA, Hunt C, Young G, Wolffsohn J. Factors affecting corneoscleral topography. Invest Ophthalmol Vis Sci. 2013 May 1;54:3691-3701.
5. Ritzmann M, Caroline PJ, Börret R, Korszen E. An analysis of anterior scleral shape and its role in the design and fitting of scleral contact lenses. Cont Lens Anterior Eye. 2018 Apr;41:205-213.
6. Van der Worp E. Speed Date – CL-SAG meets OC-SAG: part I. Global Contact. 2015;68:34-35.
7. Van der Worp E. Reaching for the Stars. Global Contact. 2017;70:30-32.
8. Harkness BM. Comparison of Sagittal Height Measurement Methods and Predicting Central Clearance for Scleral Contact Lenses. Masters thesis, Pacific University. 2015.
9. Michaud L, Tremblay C, Grégoire S, van der Worp E, Wolffsohn J, Mertz C. Relationship between Ocular Sagittal Height and Soft Contact Lens Sagittal Depth to Improve Fitting and Comfort. Poster presented at the American Academy of Optometry meeting, Chicago. 2017 Oct.
10. Kern D. Pentacam CSP data, average OC-SAG data between flat and steep meridian. Oculus. 2018.
11. Dutta D, Amankwah C, Almasyabi J. Do Standard Soft Lenses Fit Well on Out-of-Standard Eyes? Poster presented at the American Academy of Optometry meeting, Indianapolis. 2024 Nov 6-9.
12. Rojas J, van der Worp E, Pin˜ero D. OC-SAG values in 360 degrees. Poster presented at the Global Specialty Lens Symposium, Las Vegas. 2024 Jan 17-20.
13. Rodríguez-Farfach FE, Ortiz-Peregrina S, Ghinea R. Changing the paradigm of soft contact lenses fitting by sagittal height. Coopervision Optistudent Award Presentation, University of Granada (Spain), Budapest, Hungary. 2023 Sept. 16.
14. Berbegal V, Batres L, Carracedo G. Sagitta calculator software validation for soft contact lens fitting. Poster presented at the Global Specialty Lens Symposium, Las Vegas. 2024 Jan 17-20.
15. Rojas J, van der Worp E, Piñero D. OC-SAG values in 360 degrees. Poster presented at the Global Specialty Lens Symposium, Las Vegas. 2024 Jan 17-20.
16. Gundel RE, Cohen HI, DiVergilio D. Peripheral Keratometry and Soft Lens Fitting. Int Eyecare. 1986 Dec;2:611-613.
17. Young G. Ocular sagittal height and soft contact lens fit. J BCLA. 1992;15:45-49.
18. Van der Worp E, Lampa M, Kinoshita B, Fujimoto MJ, Coldrick BJ, Caroline P. Variation in sag values in daily disposable, reusable and toric soft contact lenses. Cont Lens Anterior Eye. 2021 Dec;44:101386.
19. Van der Worp E, Mertz C. Sagittal height differences of frequent replacement silicone hydrogel contact lenses. Cont Lens Anterior Eye. 2015 Jun;38:157-162.
20. Fujimoto MJ, van der Worp E, Kinoshita B, Lampa M, Coldrick BJ, Caroline P. Daily disposable soft lens sagittal depth and other lens parameter changes measured at room temperature (20 °C) and on-eye temperature (34 °C). Cont Lens Anterior Eye. 2024 Jun;47:102160.
21. ISO. Ophthalmic Optics—Contact Lenses - Part 2: Tolerances. Available at iso.org/standard/66339.html. Accessed 2024 Sep 18.
22. Young G, Hall L, Sulley A, Osborn-Lorenz K, Wolffsohn JS. Inter-relationship of Soft Contact Lens Diameter, Base Curve Radius, and Fit. Optom Vis Sci. 2017 Apr; 94:458-465.
23. Andrew M, Zimmerman A, Bailey MD. Contact Lens Adverse Events and Corneal Sagittal Depth. Invest Ophthalmol Vis Sci. 2024 Jun;65:3294.
24. Andrew M, Zimmerman A, Van der Worp E, Bailey M. The Relationship between Soft Contact Lens Movement and Relative Sagittal Depth. Poster to be presented at the American Academy of Optometry meeting, Indianapolis. 2024 Nov 6-9.
25. Chung J, Bailey M. Contact Lens Discontinuation in Presbyopia and Corneal Sagittal Depth. Poster to be presented at the American Academy of Optometry meeting, Indianapolis. 2024 Nov. 6-9.
26. Plainis S, Charman WN. On-eye power characteristics of soft contact lenses. Optom Vis Sci. 1998 Jan;75:44-54.
27. Abass A, Stuart S, Lopes BT, et al. Simulated optical performance of soft contact lenses on the eye. PLoS One. 2019 May 14;14:e0216484.
28. Van der Worp E, Montani G. Powerful Profiles. Contact Lens Spectrum. 2023 Apr;38:38-42. Available at clspectrum.com/issues/2023/april/powerful-profiles. Accessed 2024 Sep 17.
29. Van der Worp E, Bornman D, Ferreira DL, Faria-Ribeiro M, Garcia-Porta N, González-Meijome JM. Modern scleral contact lenses: A review. Cont Lens Anterior Eye. 2014 Aug;37:240-250.