
The patient is a 72-year-old female who had a late endothelial cell failure OD after 16 years and successive graft failures.
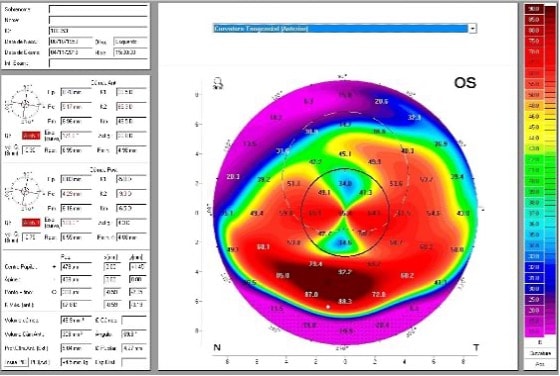
Upon examination, she presented with pellucid marginal degeneration (PMD) in her left eye (Figures 2 and 3). The patient was previously seen by a surgeon who performed an intracorneal ring implant that did not improve her vision. She opted for scleral lens fitting instead of undergoing another surgical attempt. The first attempt to fit her with a scleral lens resulted in significant touch at the lower peripheral cornea that caused discomfort and ocular hyperemia. She was then referred to our clinic, where she was successfully refit with a scleral lens in 2015.

Customized Full Scleral Lens Fitting
In February 2025, the patient returned to our clinic for care. During the pandemic, the patient was seen elsewhere, and was fit with a 17.0 mm scleral lens, which was smaller than her previous, successfully fit lens. Assessment of this lens revealed mild corneal touch around the lower cornea (Figure 4). The lens also created compression and uneven distribution at the landing zone haptic (Figure 5). The patient was unable to wear it for more than 3 hours. Additionally, the lens power had not been updated following cataract surgery a year earlier.


At this visit, corneal ectasia progression was observed. Images were utilized from slit lamp, optical coherence tomography (OCT) and anterior tomography maps and artificial intelligence (AI) to plan the new design with different angles at the haptic to achieve a smooth landing. This fit offered approximately 150 microns of clearance at the apex and reduced the excessive superior vaulting of previous lenses by designing a reverse aspheric anterior and posterior design to minimize lens mass. A posterior oval microvault was added to prevent touch on the apex and non-visible ventilating channels at the haptic to increase oxygen delivery (Figures 6 and 7). Scleral lens parameters were:
Lens parameters include a base curve 45x48 D / 7.50 mm x 7.03 mm; power –0.50 D; overall diameter 20.5 mm; optic zone 9.0/14.0, sagittal height 9.110; oval microvault at 10.0 mm to 12.5 mm at 6 o’clock; and 200-Dk material.


Conclusion
The patient reported comfort and a calm eye after 10 to 12 hours of lens wear. This case highlights the efficacy of tailored scleral lens designs, incorporating microvaults and ventilation, for managing complex, progressive PMD.
References
- Asena L, Altınörs DD. Clinical outcomes of scleral Misa lenses for visual rehabilitation in patients with pellucid marginal degeneration. Cont Lens Anterior Eye. 2016;39(6):420-424. doi:10.1016/j.clae.2016.06.010
- Bézé S, Benoist d’Azy C, Lambert C, Chiambaretta F. Efficacy of visual rehabilitation of patients with pellucid marginal degeneration fitted with SPOT® scleral contact lenses. J Fr Ophtalmol. 2020;43(1):e1-e5. doi:10.1016/j.jfo.2019.11.004
- Rathi VM, Dumpati S, Mandathara PS, Taneja MM, Sangwan VS. Scleral contact lenses in the management of pellucid marginal degeneration. Cont Lens Anterior Eye. 2016;39(3):217-220. doi:10.1016/j.clae.2015.11.005
- Dutta R, Iyer G, Srinivasan B, Iqbal A. Aberration change after scleral lens wear in eyes with pellucid marginal degenerations. Indian J Ophthalmol. 2024;72(7):1037-1042. doi:10.4103/IJO.IJO_1820_23
- Cunningham B. Clinical findings and management of pellucid marginal degeneration using scleral lenses over INTACS and corneal collagen cross-linking with riboflavin. JCLRS. 2018;2(1):e1-e14. doi: 10.22374/jclrs.v2i1.13
- Barone V, Petrini D, Nunziata S, et al. Impact of scleral lenses on visual acuity and ocular aberrations in corneal ectasia: A comprehensive review. J Pers Med. 2024;14(10):263. doi: 10.3390/jpm14101051
- Fadel D. Three of a Kind: Examples of challenges presented with scleral lens patients and how to overcome them. Contact Lens Spectrum. 2023;38(7):32-36, 38-40, 51. clspectrum.com/issues/2023/july/three-of-a-kind



