An existing scleral patient referred his 81-year-old grandmother with advanced keratoconus (KCN) and compromised vision to our office after being advised by her previous provider that there was nothing more they could do to improve her vision.
Case Description
She presented with advanced stage KCN and a history of a full-thickness corneal transplant OD. She had worn a GP lens for many decades, and wanted to see if any improvement could be made with her vision and comfort. Chief complaint was blurry vision OU, with uncorrected visual acuity OD count fingers, OS count fingers with no improvement on pinhole. Habitual corneal GP’s VA was 20/400 OD and 20/200 OS. Keratometry was 51.25 @ 89 / 57.50 @ 179 OD, and 43.25 @ 003 / 46.50 @ 093 OS, with auto-refraction of -7.75 -16.25 x 93 OD and -1.50 -2.75 x002 OS. Topography revealed advanced keratoconus, especially in the right eye.
Her right eye initially fit empirically, and we were able to correct her to 20/100. She had a dense 4+ nuclear/ PSC cataract in each eye that would not improve on pinhole. Therefore, the patient was referred for cataract surgery in OD with the plan to afterwards refit into scleral lenses.
Upon revisiting the office, she was wearing her corneal GPs being unable to discontinue lens wear without any other type of correction. Initial OCTs revealed central 3-point touch with inferior edge clearance. Topography measured a Best Fit Sphere (BFS) of 6.21mm and white to white (WTW) corneal size of 11.36 OD.
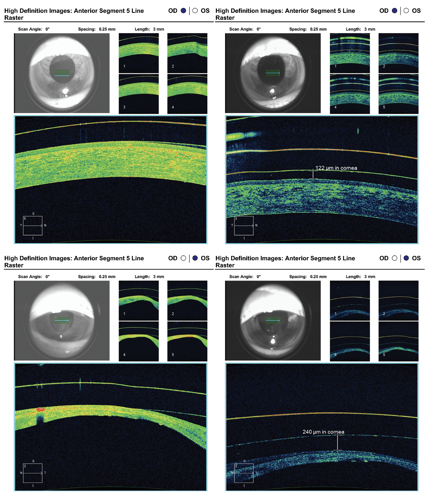
Based on empirical fitting programs, we started with a Naturalens Mini Scleral (Advanced Vision Technologies). The initial dispense revealed 6mm of central touch and an over-refraction of -6.50 -1.50 x 175. We increased the vault of the initial lens by 500 microns (µm) adjusting the power accordingly. On second dispense she still had a -1.00 -.75 x 165 O/R with 176µm of clearance. The haptic zone was toric standard by half flat with no billowing or blanching. The third lens was even better, with good vision 20/80 and clearance. However, she finally decided to have cataract surgery a month later for her right eye, and the power was adjusted downward based on the new implant. We also had to increase the sagittal depth to account for the corneal rebounding after switching from GPs to sclerals.
Her cataract surgeon recommended penetrating keratoplasty (PKP) before cataract surgery in her left eye due to her thin cornea. However, she decided not to proceed, so we refit the left eye with an empirical fit. The initial lens was touching 4mm centrally, so the sag was increased 300µm while adjusting BC and power. On second dispense, the haptic zone was flattened by half, and eventually increased her sag due to the cornea rebounding. We were able to adjust the power to achieve 20/70 OS with 244µm of clearance.
Discussion
With only a couple of follow-up visits, this patient was best corrected to 20/40 OD and 20/70 OS. The left cornea was so thin that cataract surgery was considered high risk and she did not want to go through with a PKP OS. Despite all these factors, she is still able to see 20/40 OU and has been thrilled with her life-altering vision.
Conclusion
This was a very challenging, yet rewarding, scleral lens refit. Although there was difficulty with application and removal, the net result was better vision, comfort, and improved lifestyle.
Benjamin Teller, OD, is founder of EyeRx in Chevy Chase, MD, and is a member of the National Eye Advisory Council. He has no disclosures to report.



