A 59-year-old female presented to our specialty contact lens service referred by her cornea specialist for scleral lens evaluation.
Case Description
This patient has an extensive ocular history of keratoconus in both eyes, and had originally undergone penetrating keratoplasty in both eyes at least 14 years ago. After a suture removal procedure following the corneal transplantation surgery, the patient developed Candida endophthalmitis in her left eye and later Streptococcus oralis with endophthalmitis in the same eye.
After complete resolution from these infections, the patient underwent a combined procedure of repeat corneal transplantation and cataract extraction with posterior chamber intraocular lens placement in the left eye. The patient later developed glaucoma in both eyes, which required glaucoma surgeries (glaucoma drainage tube placement on the right eye and trabeculectomy surgery on the left) to better control her intraocular pressures. With an updated glasses prescription after surgery, her visual acuity in the right eye fluctuated between 20/200 and 20/60 with a manifest refraction of -5.00 -6.00 x 075, and the visual acuity in the left eye fluctuated between 20/80 and 20/40 with a manifest refraction of +7.00 -7.00 x 120.
The patient presented to our clinic looking for an alternative specialty contact lens. Her goals were to improve visual acuity, improve ocular dryness symptoms, and protect the ocular surface. The patient was using topical prednisolone acetate twice daily in the right eye, topical loteprednol etabonate three times daily in the left eye, topical cyclosporine 0.05% twice daily in both eyes, and preservative-free artificial tears as needed.
The patient was previously fit into corneal GP lenses, hybrid contact lenses, and free-form scleral lenses. Unfortunately, all these options provided poor comfort and the patient became intolerant. The patient reported that with the most recent pair of lenses (free-form scleral lenses), her vision was good at the time of lens application but did not stay clear during the day, describing that within 4 hours of scleral lens wear time her vision would become foggy and her eyes would become very red and irritated (in the left eye more than the right). Her previous specialty lens provider attributed the decrease in visual acuity to development of corneal edema and advised the patient to limit her wear time with these lenses. The patient was frustrated with her visual limitations, as they were affecting her ability to complete her daily work.
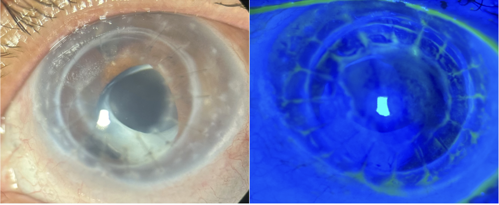
At our consultation, we extensively discussed realistic goals and expectations. We decided to refit both eyes with BostonSight SCLERAL lenses because of the available SmartChannel technology, which helps mitigate suction and edema that may result from scleral lens suction. The first two trial lens attempts provided better ocular comfort, but the patient was still developing microcystic corneal edema after 5 to 6 hours of wear time. The patient also described having a more challenging time removing her left lens at the end of the day. At each evaluation, intraocular pressures were measured after lens removal and were always adequate and within normal range.
Discussion
To aid in bringing more oxygen to the cornea, and help accommodate for previous glaucoma surgeries while minimizing scleral lens suction, one wide channel was incorporated in the superior-temporal aspects of each lens. With the addition of these channels, the patient noticed further improvement in comfort and can wear the lenses with almost complete resolution of corneal microcystic edema. No staining has been noted on her cornea or conjunctiva after lens removal, and her best-corrected visual acuities with lenses are stable at 20/25 OD and 20/25 OS.
_________
Dr. Sotomayor is senior optometrist at Bascom Palmer Eye Institute in Florida. She is a Fellow of the Scleral Lens Education Society. She has received honoraria from Boston Sight.



