Approaches to scleral lens use have changed dramatically. A scleral contact lens is no longer a device that just improves vision, but a device that can help regulate the ocular ecosystem.
Case Description
A 45-year-old male was suffering from severe left eye pain with the presence of persistent corneal epithelial defect (PCED) and a corneal ulcer 2 mm in diameter. He previously had cataract surgery in both eyes, followed by recurrent ulcer and PCED OS, and therapeutic management with a soft contact lens had been started.
The corneal ulcer and left eye de-epithelialization was managed with pharmacological treatment of an antibiotic, an anti-inflammatory, and an ocular lubricant. His glaucoma was managed with a carbonic anhydrase inhibitor (Azopt, Novartis) and a beta-blocker (timolol).
In November 2023, the patient described mild pain and foreign body sensation OS. Two months later, he presented with moderate pain in both eyes while seeing only shadows in his left eye since December 2019. Corneal decompensation was noted with the presence of bullae, leukoma, and central corneal ulcer (2 mm) OS. He also described losing vision and the presence of inferior temporal ulcer (1 mm) in his left eye, and continued with pharmacological treatment.
In June 2024, the patient was referred for fitting of a specialized contact lens due to constant pain OS (intense) and OD (mild). The objective was to reduce the pain, promote corneal tissue regeneration, and avoid possible graft rejection in the short term.
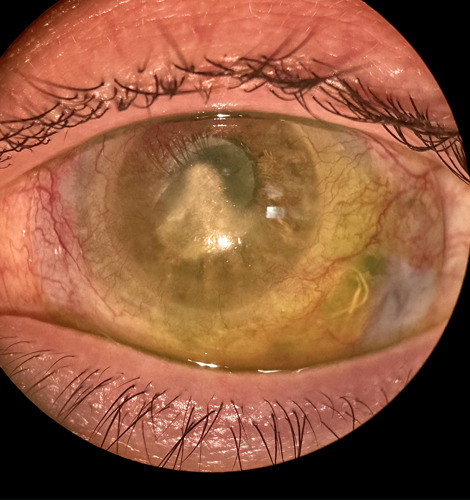
A slit-lamp examination showed corneal decompensation with the presence of leukoma, PCED, and a corneal ulcer (2 mm diameter) in the right eye (Figure 1), while the left eye showed mild de-epithelialization.
Best-corrected visual acuity (BCVA) in the right eye was light perception and in the left eye was 20/80 with reduced visual field.
Keratograph analysis was performed, with meibography measuring meibomian gland dysfunction (MGD) of 2° OD and 3° OS. The noninvasive tear breakup time was 2 seconds OD and 0 seconds OS.
The deterioration of the corneal surface did not allow tomography acquisition or specular microscopy to determine the status of the corneal endothelium.
The presence of ocular surface disease was observed with MGD and subsequent PCED and corneal ulcer. Possibly, chronic use of glaucoma medications may also have had implications for PCED (Figure 1).
As management, the Maxim 3D scleral lens (Acculens) was prescribed for the left eye. The parameters are as follows: diameter 18.2 mm, base curve 44.00 D (5500 µm), toric haptics (400 µm/300 µm), Dk 180, Hydra-PEG treatment.
Upon return to the office, and 1 hour after lens insertion, the lens was observed to be centered, with a smooth scleral support and a low clearance of approximately 150 µm.
The patient stated that the lens was comfortable and he did not feel pain in the left eye.
Therapeutic management was complemented with autologous serum to promote corneal re-epithelialization.
During a 3-week followup visit, a practically recovered epithelium was observed and the patient was able to carry out his activities normally.
Discussion
The use of scleral lens is recommended in these cases, with favorable results in the recovery of the corneal epithelium and attenuation or suppression of the present symptomatology, such as pain and photophobia.
Autologous serum is shown to be an important adjunct in the treatment of PCED by accelerating the corneal re-epithelialization process.
Patients using scleral lenses in ocular surface disease undergo a positive change with a great impact on their quality of life and visual quality, allowing them to regain functionality in various activities at work and socially.
--------------
Dr. Carmona, based in Peru, is a specialist in the treatment of ocular surface disease and scleral lens fitting. He is a paid speaker for Acculens and Alcon.



