Salzmann’s Nodular Degeneration (SND) is a progressive, non-inflammatory corneal condition commonly found in middle-aged females. It is characterized by the appearance of gray-white elevated nodules near the corneal midperiphery/limbus, which creates an obstruction and challenge for the fitting of scleral lenses. These nodules also can lead to increased irregular astigmatism and reduced visual acuity (VA). Treatment options can vary from topical treatments, such as artificial tears, steroids and customizable scleral lenses, to surgical options such as phototherapeutic keratectomy.
Case Description
A 59-year-old Caucasian female was referred for a specialty lens consult secondary to SND. She also had irregular astigmatism, ocular surface disease (OSD), and mild cataracts with longstanding symptoms of reduced VA and depth perception, glare at night, foreign body sensation, and dry eye. Her current glasses improved her VA slightly but did not alleviate visual disturbances. Current medical treatments included lifitegrast and preservative-free artificial tears. Due to her persistent symptoms, her referring doctor was considering surgery, but suggested a specialty lens consult prior to proceeding with surgery.
Her entering VA with her current correction (spectacles) was 20/25 OD and 20/25-2 OS; an updated refraction (+0.50 -0.75 X 061 OD, +0.72 -1.25 X 123 OS) did not yield any improvement, and distortion persisted.
A slit-lamp exam revealed meibomian gland dysfunction OD and OS, large elevated nodules at the superior-nasal limbus with iron deposits OS>OD, trace central punctate epithelial erosions OD and OS, and mild age-related cataracts OD and OS.
Scleral lenses appeared to be the best option to provide improved VA and comfort. One challenge that emerged during the fitting was the large peripheral nodules; thus, we needed a lens to vault over the nodules without overvaulting the rest of her limbus. Due to its many customizable features, including the ability to adjust the limbal zone in four independent quadrants, we proceeded with the Onefit MED+ (Blanchard/CooperVision) scleral lens in BostonXO2.
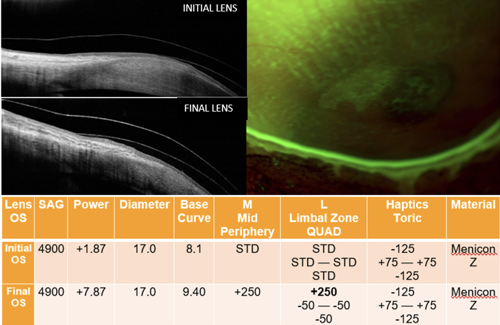
The initial OS lens provided significant improvement in the quality of vision and ocular comfort. While the rest of the lens was fitting well, there was touch at her peripheral corneal nodules OU, confirmed with OCT scans. The post-lens assessment showed sodium fluorescein (NaFl) stain.
The OCT images showed touch in the superior nasal region starting from the midperiphery (M zone) all the way through the limbus (L zone). To correct this, we first increased our M zone by 250 µm (no SAG change). We increased our L zone by another 250 µm in just the superior quadrant and decreased the L zone in the other 3 quadrants by 50 µm to avoid overvaulting the rest of the limbus. Similar changes were made for the OD lens.
The changes we incorporated in the M zone and individual L zones were successful (Figure 1). After 6 hours of wear, her central vault, haptics, midperiphery, and limbal regions were all fitting well with no touch at her nodules. Her post-lens assessment also showed no signs of NaFl staining or lens touch of the nodules and was confirmed at max wear time. Her VA was 20/20 in each eye and she had no over-refraction.
Discussion
In recent years, scleral lenses have emerged as a successful option to manage patients with SND. Long-term, the ocular surface is protected from external irritants, and the progression is potentially slowed. To provide a proper scleral lens fit over the large nodules found in SND patients, a customizable design is necessary. In this case, modifying both the mid-corneal region and quadrant-specific limbal design provided the optimal solution for our patient.
_________
Dr. Hemmati is the founder and clinic director of the Austin Contact Lens Institute in Austin, TX. She is a Fellow in the American Academy of Optometry. She is a compensated KOL and/or speaker for CooperVision and Euclid.



