As scleral lens designs are advancing, customizable parameters are becoming more specialized. Difficult-to-fit corneas with significant asymmetries quadrant by quadrant are more easily matched without under- or overvaulting. Since previous studies have confirmed that the majority of patients have toric scleral profiles,1,2 the industry originally shifted toward providing toric landing zones to account for these new data.
Case Description
A 37-year-old male patient with keratoconus presented for scleral lens evaluation after experiencing a lengthy red-eye event after sleeping in his habitual scleral lenses. The patient was originally evaluated at the emergency visit and 4 subsequent follow-up visits by his corneal specialist during the 2 months preceding the contact lens evaluation visit.
His scleral lenses appeared to be applanating at least 3 mm in both eyes with severe overvaulting at the limbus 360°, as well as significant decentration. Corneal findings included central scarring, apical thinning, 2+ diffuse superior punctate keratitis with additional 3+ sodium fluorescein staining centrally and along the limbus, and 1+ microcystic edema along the limbus. Incoming visual acuity was 20/80 OD and 20/60 OS.
We opted to refit the patient. The patient’s new corneal topography revealed areas of central flattening from the scleral lens compressing the cornea for an unknown period of time. This new reverse geometry–appearing corneal topography was likely going to regress somewhat as the cornea rehabilitated itself to its new natural shape.
Over the course of 3 months, repeated corneal topography scans were taken until the patient’s cornea stabilized. During this time period, new scleral lens fitting was initiated with the Delta Scleral lens (ABB Optical). The lens fit was initially overvaulted in all regions to give the patient’s cornea space to rehabilitate and then lowered as the patient’s cornea stabilized to more acceptable clearance values. The patient’s lens wear time was strongly limited during this timeframe, and he was asked to refill the lens at least once halfway through the day.
Eventually, the lens fit improved with the incorporation of 2 different sagittal depths in the bowl of the lens. Essentially acting as a bitoric design, the new lenses were significantly better centered, and the limbal clearance was much improved. Eventually, the patient’s final visual acuity was 20/60 OD and 20/70 OS. The microcystic edema and superior punctate keratitis were completely resolved by the last follow-up visit.
Discussion
As scleral lens designs improve the ease of fitting for the practitioner and the overall scleral lens fit, choosing a lens design that best suits the patient’s needs is imperative. For the average practitioner who does not have advanced imaging technology or access to specialized scleral lens fitting in the form of impression-based scleral lenses, opting for scleral lens designs can streamline fit and improve the fitting process.
Conclusion
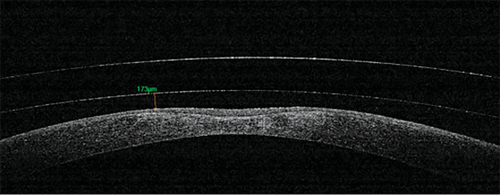
The patient’s previous best corrected visual acuity was OD 20/25 OD and 20/25 OS. With poorly fitting lenses that had been chronically applanating the patient’s cornea, the patient had resultant corneal scarring and corneal thinning that resulted in irreversible vision loss (see Figure 1).
References
- Visser ES, Visser R, van Lier HJJ. Advantages of toric scleral lenses. Optom Vis Sci. 2006;83(4):233-236.
- Visser ES, Visser R, van Lier HJJ, Otten HM. Modern scleral lenses part II: patient satisfaction. Eye Contact Lens. 2007;33(1):21-25.
To hear Dr. Song discuss this case, click here.




