Scleral lenses have emerged as a valuable therapeutic tool in the care of compromised corneas, offering optical rehabilitation and ocular surface protection. This case report describes rehabilitation of a patient with a failing penetrating keratoplasty (PK) graft using a customized scleral lens fabricated from a high Dk material.
Case Description
A 68-year-old female patient with a history of PK in the left eye presented with progressive visual decline and glare. She had previously worn a scleral lens with moderate success but reported worsening image quality, photophobia, decreased lens wear tolerance, and reduced functional vision. At presentation, best-corrected visual acuity (BCVA) in the left eye was hand motion.
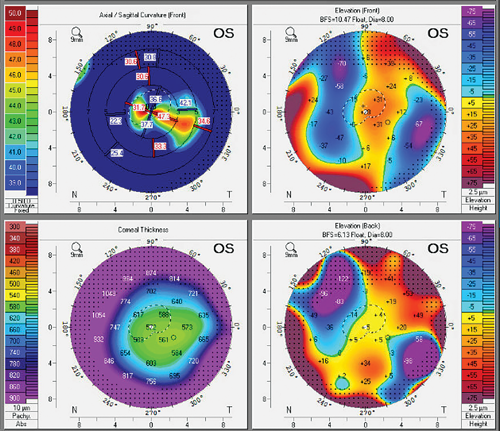
Slit lamp examination revealed diffuse stromal haze and epithelial microcystic edema, consistent with endothelial cell failure and graft decompensation. The cornea appeared thickened with an irregular contour. Corneal tomography confirmed central edema, an elevated posterior float, and irregular astigmatism.1,2 The existing scleral lens failed to maintain a stable fluid reservoir and did not provide adequate optical performance or central clearance.
In coordination with the patient’s cornea specialist, the clinical approach was to improve oxygen delivery to reduce edema and support graft viability.3,4 A scleral lens fabricated from Optimum Infinite (Contamac), a hyper-Dk material, was chosen for oxygen permeability. While the material’s wetting properties aided optics, oxygen delivery to the stressed cornea was the priority.1,3 Improved surface wettability was an additional advantage that contributed to visual rehabilitation by maintaining a smooth, continuous tear film across the lens surface.
A 14.9 mm oblate lens design was chosen for the irregular post-PK corneal shape.2,5 Toric peripheral curves and customized edge lift zones were chosen to optimize scleral alignment, enhance limbal clearance, and reduce localized compression.
Discussion
Initial lens performance demonstrated central clearance without corneal bearing, and further refinements improved centration and edge alignment. Following 2 design modifications, the final lens achieved uniform vault, stable peripheral landing, and reduced midday fogging. The patient reported improved vision and more consistent performance throughout the day.
After 4 weeks of regular wear and concurrent topical therapy, BCVA improved to 20/150 in the left eye. Subjective symptoms such as glare and fluctuating vision decreased. Tomography showed reduced central corneal thickness and improved epithelial contour, signifying less edema and enhanced stability.1,2
Conclusion
This case demonstrates that in the presence of endothelial decompensation, maximizing oxygen permeability becomes critical for maintaining corneal clarity and prolonging surgical intervention.3,4 Combining a high Dk material with a customized lens design allowed for both therapeutic and visual benefits in an eye at risk of failure.
References
- Michaud L, van der Worp E, Brazeau D, Warde R, Giasson CJ. Predicting estimates of oxygen transmissibility for scleral lenses. Cont Lens Anterior Eye. 2012;35(6):266-271. doi:10.1016/j.clae.2012.07.004
- Visser ES, Visser R, van Lier HJJ, Otten HM. Modern scleral lenses part 1: clinical features. Eye Contact Lens. 2007;33(1):13-20. doi:10.1097/01.icl.0000240045.47742.1f
- Conditions NRC (US) WG on CLUUA, Flattau PE. Hypoxia [Internet]. www.ncbi.nlm.nih.gov. National Academies Press (US); 1991. Available from: https://www.ncbi.nlm.nih.gov/books/NBK234101/
- Pullum KW, Buckley RJ. A study of 530 patients referred for rigid gas permeable scleral contact lens assessment. Cornea. 1997;16(6):612-622. doi:10.1097/00003226-199711000-00008
- Summers B. Fitting the Surgically Compromised Cornea [Internet]. Revieweducationgroup.com. Review of Optometry; 2018 [cited 2025 Aug 11]. Available from: https://www.revieweducationgroup.com/ce/fitting-the-surgically-compromised-cornea1
To hear Dr. Eaves discuss this case, click here.




