For one patient, insomnia became so severe she was hospitalized after 9 consecutive sleepless nights. This case report highlights the connection between chronic insomnia and ocular surface disease, shedding light on how scleral lenses can help
restore vision and sleep quality.
Case Description
A 24-year-old female patient presented with ghosted vision and difficulty reading small print. Her medical history included type 1 diabetes mellitus (19 years), chronic insomnia (8 years), and depressive disorder.
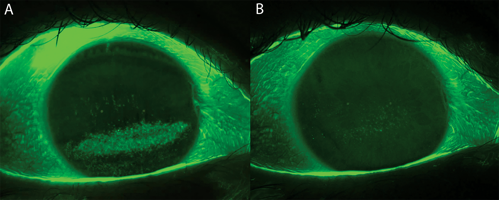
Visual acuity with eyeglasses was 20/25 OD and OS. Slit lamp examination with vital dyes revealed exposure keratopathy and trace perilimbal conjunctival dryness OD and OS. Corneal sensitivity was reduced OD and OS, and she denied ocular pain. Corneal topography revealed inferior steepening OU with K readings of 44.80/47.89@090 OD and 44.90/47.52@073 OS. Pachymetry showed localized thinning with a minimum corneal thickness of 459 µm OD and 469 µm OS.
The patient was diagnosed with neurotrophic keratopathy and limbal stem cell fatigue from chronic exposure. When questioned further about sleep habits, she denied sleeping with her eyes open. Despite taking zaleplon nightly, she averaged only 3 to 4 hours of sleep. In 2018, she was hospitalized and required high-dose sedatives after 9 sleepless nights.
To restore corneal integrity and vision, the patient was fitted with Ampleye (Art Optical Contact Lens, Inc.) scleral lenses. The 15.5-mm diameter lenses were selected because of her small visible iris diameters of 11.1 mm, and 3,600 µm of sagittal depth provided adequate vault over her cornea and limbus. The standard 125-µm toric haptic aligned well to her sclera. Optimum Infinite material was selected to enhance oxygen transmissibility, and a PEG coating was added for better wettability.
While awaiting the scleral lenses, bandage soft contact lenses (8.4/Plano/14.0) were fitted to mask her irregular astigmatism and provide functional vision. However, the lenses decentered significantly temporal secondary to the elevated nasal conjunctiva/sclera. Switching to larger-diameter, lower-modulus daily disposable lenses (8.5 base curve/14.3 diameter) improved centration, vision, and comfort. She was also prescribed preservative-free artificial tears to be administered hourly during the day and lubricant eye ointment, eyelid taping, and moisture-chamber goggles to be used at night.
At her scleral lens follow-up, she reported discovering that she did, in fact, sleep with her eyes slightly open. Her vision and corneal topography normalized within 3 months, and her quality of life greatly improved. Combined therapy with scleral lenses and nighttime lubrication allowed her to sleep regularly for the first time in years. The patient was extremely pleased to find the “cure” for her insomnia.
Discussion
Nocturnal lagophthalmos is a lesser-known contributor and often goes undetected in patients with reduced corneal sensation. Without proper intervention, this can silently lead to corneal epithelial breakdown, ulceration, and even perforation.1
This case illustrates how an insidious ocular condition can manifest as systemic sleep disturbance. Scleral lenses can significantly improve quality of life for patients with concurrent exposure-related keratopathy and insomnia.
References
- Tsai SH, Yeh S-I Chen L-J, Wu C-H, Liao S-L. Nocturnal Lagophthalmos. Int J Gerontol. 2009;3(2):89-85. doi:10.1016/S1873-9598(09)70027-4
To hear Dr. Avisado discuss this case, click here.




